
An X-ray of a knee joint affected by an avulsion fracture where the ligament tore a part of the bone away from the knee.
The April 2017 issue of the Journal of the American Academy of Orthopedic Surgeons features a compelling review article covering the topic of lower extremity avulsion fractures in pediatric and adolescent athletes. Drs. Jonathan Schiller, Steven DeFroda and Travis Blood discuss the effects of misdiagnosing lower extremity avulsion fractures. Avulsion fractures are more common in adolescents and happen when there is an injury to the bone in a place where a tendon or ligament is attached. The fracture causes the tendon or ligament to pull off a piece of bone.
Types of Avulsion Fractures
The JAAOS article discusses the most common places where the pediatric athlete will get avulsion fractures. The pediatric athlete has growth plates that are still open and attached to the tendon. Typically the growth plate is weak and when there is a traumatic event, the plate can often suffer an avulsion fracture.
The most common places where pediatric patients will have avulsion fractures are at the anterior superior iliac spine and the anterior inferior iliac spine along with the ischial tuberosity. It is extremely important for medical professionals to conduct a plain x-ray when physically examining a patient in this case. The physical examination could be consistent with a muscle strain or apophysitis. Apophysitis tend to occur with overuse whereas an avulsion fracture tends to happen acutely. The athlete may describe a popping sensation at the time of the injury.
Another avulsion fracture, tibial tubercle avulsion, is not very common, but requires immediate surgical fixation. A healthcare provider should be quite cognizant if their patient comes in with knee pain that could perhaps be the result of a tibial tubercle avulsion fracture.
How to Treat Avulsion Fractures
The most common way to diagnose an avulsion fracture is by x-ray. However, other injuries may require the use of a CT scan or MRI. CT imaging is more commonly used in the case of a tibial tubercle avulsion fracture. In general, treatment for this type of avulsion fracture is conservative unless there is a significant amount of displacement.
Nonsurgical treatment is divided up into a five stage protocol, which consists of:
- Ice, rest, anti-inflammatories for the first week of the injury
- From week one to week three, involves gentle passive range of motion and assisted partial weightbearing is performed
- Resistance training occurs
- Allows aggressive stretching and sport specific activity after one to two months
- Two months post injury when the athletes are returned back to sports without restriction
Ischial Tuberosity
The ischial tuberosity is the origin of the hamstring muscles which involve the long head of the biceps femoris, semitendinosus and semimembranosus. Avulsion fractures in this area are caused by a forceful flexion of the hip joint and extension at the knee. It typically takes place during sprinting or kicking. If the avulsion fracture is displaced more than 15 mm, surgery is recommended.
Anterior Superior Iliac Spine
These fractures are secondary to increased force from the sartorius and tensor fascia lata. They both originate from the anterior superior iliac spine. Nonsurgical management is recommended except if displacement is greater than 2 cm. These typically occur as a result of sudden straining, twisting, such as in baseball, jumping, and sprinting.
Anterior Inferior Iliac Spine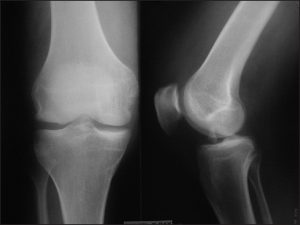
AIIS fractures are secondary to an increased force from the rectus femoris. AIIS injuries typically occur during forceful hip hyper-extension and knee flexion. Conservative treatment is recommended for these avulsion fractures unless displacement is greater than 2 cm.
Pubic Synthesis and Iliac Crest
These avulsion fractures are rare and occur from increased activity or force from adductor tendons, which originate from the pubic synthesis. These tend to occur during kicking type activity. An MRI scan is typically needed to facilitate a diagnosis in this area. The rectus abdominis muscles attached to the iliac crest and avulsion fractures can occur during forceful turning or lateral flexion of the area. If the fracture is greater than 3 cm of displacement, surgery would be recommended.
Tibial Tubercle
These fractures occur with forceful contraction of the quadriceps. It is important to quickly diagnose this particular injury because nonsurgical treatment is not only ineffective, but can also cause the lower extremity to become dysfunctional. X-rays are sufficient to make the initial diagnosis, but CT scans are able to better classify the extent of the injury. Because of the strong contraction of the quadriceps causing fracture displacement, these injuries rarely heal without surgical intervention.
Greater Trochanteric
Fractures of the hip are rare in the pediatric population and are typically encountered in obese patients. This type occurs with the hip in flexion and with external rotation. Nonsurgical treatment is recommended for all trochanteric fractures. Surgery should be considered if there was significant displacement at the site of the fracture greater than 2 cm.
If you are feeling any significant pain in your joints, regardless of if you are an athlete or not, visit Dr. Stacie Grossfeld of Orthopaedic Specialists, PLLC in Louisville, KY. With the help of Dr. Grossfeld, you can prevent further damage to your ligaments, joints, and bones while starting a treatment plan to fix any existing damage. Contact Dr. Grossfeld here or by calling 502-212-2663 today!

 Coronary Heart Disease (CHD) is the most common type of heart disease to affect Americans and is also the type of heart disease that people are most likely to be talking about when discussing heart disease. CHD occurs when plaque builds up in the coronary arteries. Coronary arteries are the enlarged veins that move blood into the heart. When plaque builds up in these arteries, they narrow and less blood is able to travel to the heart. Narrowed arteries and less blood flow increase the risk of heart attack or chest pain which means it is very important to keep your heart healthy and avoid heart disease.
Coronary Heart Disease (CHD) is the most common type of heart disease to affect Americans and is also the type of heart disease that people are most likely to be talking about when discussing heart disease. CHD occurs when plaque builds up in the coronary arteries. Coronary arteries are the enlarged veins that move blood into the heart. When plaque builds up in these arteries, they narrow and less blood is able to travel to the heart. Narrowed arteries and less blood flow increase the risk of heart attack or chest pain which means it is very important to keep your heart healthy and avoid heart disease.


 The human elbow is an intricate part of the body. While it is essentially a hinge joint and looks fairly straightforward – the elbow is made up of a complicated series of bones, joints, and ligaments. Within the elbow the radius and ulna must rotate and slide with the humerus to bend or straighten the arm. These movements are possible with the help of ligaments and there are two main ligaments that are important in order to achieve optimal elbow maneuverability: the lateral collateral ligament and the ulnar collateral ligament.
The human elbow is an intricate part of the body. While it is essentially a hinge joint and looks fairly straightforward – the elbow is made up of a complicated series of bones, joints, and ligaments. Within the elbow the radius and ulna must rotate and slide with the humerus to bend or straighten the arm. These movements are possible with the help of ligaments and there are two main ligaments that are important in order to achieve optimal elbow maneuverability: the lateral collateral ligament and the ulnar collateral ligament. The Theory
The Theory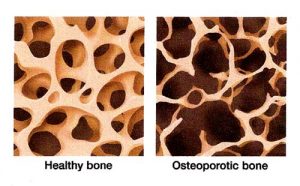 This month we are focusing on bone health. Unless you have recently sustained an injury to your bones, then it’s unlikely you’ve been putting much thought into their health. Since we can’t see our bones, it is much more difficult to remain aware and alert to their needs. For example, osteoporosis, which is a condition that degrades bones, is a common disease and yet most people aren’t aware of its serious effects on bone health.
This month we are focusing on bone health. Unless you have recently sustained an injury to your bones, then it’s unlikely you’ve been putting much thought into their health. Since we can’t see our bones, it is much more difficult to remain aware and alert to their needs. For example, osteoporosis, which is a condition that degrades bones, is a common disease and yet most people aren’t aware of its serious effects on bone health.  Many people suffer from bone marrow edema or insufficiency fractures. And the long term effects of these conditions can be serious. Edema and insufficiency fractures can injure a person’s bone marrow and cause a long list of medical complications.
Many people suffer from bone marrow edema or insufficiency fractures. And the long term effects of these conditions can be serious. Edema and insufficiency fractures can injure a person’s bone marrow and cause a long list of medical complications.
Recent Comments