The current healthcare environment in America has been driven by the concepts of quality, cost containment and value. Based on this, the federal government is starting a program that will incentivize physicians to maximize and reduce the patient’s risk factors prior to hip and knee replacement surgery. In fact, a physician’s reimbursement for the procedure will be directly related to post-surgical outcomes of their patients. Because of this, there are many studies right now looking at “tools” to predict high-risk patients to figure out if those patients should even be offered a knee replacement or if there are pre-surgical ways to reduce the risk factors.
There was an article published by Dr. David Manning in the American Academy of Orthopedic Surgeries Journal, this January. This report looked at risk prediction tools for hip and knee replacement surgery.
In this article, Dr. Manning noted that total knee 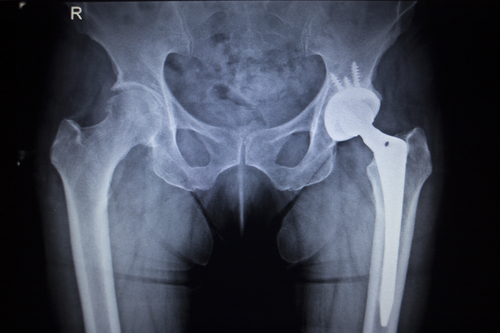 and total hip surgeries comprised a largest procedural expenditure in the Medicare budget. And the complication rate for these surgeries varies anywhere between 2 percent and 14 percent. Higher complication rates are associated with the elderly and patients with additional disorders and high risk factors. Between 1991 and 2010, the mean number of comorbidities among Medicare patients undergoing elective total knee replacement nearly doubled from 1.2 to 2.1, and this trend is expected to continue.
and total hip surgeries comprised a largest procedural expenditure in the Medicare budget. And the complication rate for these surgeries varies anywhere between 2 percent and 14 percent. Higher complication rates are associated with the elderly and patients with additional disorders and high risk factors. Between 1991 and 2010, the mean number of comorbidities among Medicare patients undergoing elective total knee replacement nearly doubled from 1.2 to 2.1, and this trend is expected to continue.
Patients treated with total knee replacement show that the rate of diabetes mellitus increased from 10.5 percent to 24.2 percent. The rate of obesity increased from 4 percent to 10 percent during the same period. Complications that are seen after total joint replacement such as infection, blood clots, heart attacks, pneumonia, are associated with poor patient outcomes, and in addition represented a substantial cost burden to the American healthcare system.
Quality Improvement Initiatives Target Total Hip and Knee Replacement Surgery
Over the next five years, elective total hip and total knee replacements will be incorporated into several quality improvement initiatives, developed by the Center for Medicare and Medicaid Services. Because risk prediction tools or risk calculations are being developed, physicians are receiving help to determine who is eligible for a knee replacement or hip surgery. It is also working to understand if those risk factors can be modified pre-surgical efforts. (more…)


 Many people experience elbow pain at some point in time. Your elbow is a somewhat complex mechanism that relies on three different bones for support and movement. The elbow gives your arm the ability to rotate outward and inward, while also working like a hinge upward and downward.
Many people experience elbow pain at some point in time. Your elbow is a somewhat complex mechanism that relies on three different bones for support and movement. The elbow gives your arm the ability to rotate outward and inward, while also working like a hinge upward and downward. Osteoarthritis and meniscal tears are injuries that both occur in the knees. Both knee injuries tend to become more probable to occur with age; however, there are significant differences between osteoarthritis and meniscal tear injuries. The pain associated with both injuries require different treatment approaches. A big factor that decides treatment is if the pain is a result of a particular injury or health factor. To understand these two distinct injuries that occur in the knees, here are 10 major differences between the two.
Osteoarthritis and meniscal tears are injuries that both occur in the knees. Both knee injuries tend to become more probable to occur with age; however, there are significant differences between osteoarthritis and meniscal tear injuries. The pain associated with both injuries require different treatment approaches. A big factor that decides treatment is if the pain is a result of a particular injury or health factor. To understand these two distinct injuries that occur in the knees, here are 10 major differences between the two.
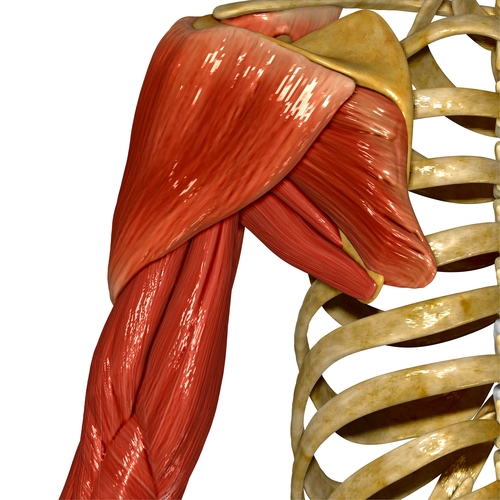 We know that rotator cuff tears commonly affect one shoulder, especially in patients who are over age 55. However, there is a group of patients that not only tear one shoulder, but end up tearing their contralateral shoulder as well. There was a study published in the
We know that rotator cuff tears commonly affect one shoulder, especially in patients who are over age 55. However, there is a group of patients that not only tear one shoulder, but end up tearing their contralateral shoulder as well. There was a study published in the  Vitamin D deficiency is epidemic that affects an estimated one billion people worldwide. This nutrient is associated with many functions and organs in your body. Research shows that insufficient levels are associated with a greater rate of heart disease and mortality. Vitamin D levels less than 20 ng/mL are associated with a risk increase to 30 to 50 percent for developing colon, prostate, and breast cancer as well as an increased mortality from these cancers. In addition, vitamin D helps to maintain the health of your bones and muscles.
Vitamin D deficiency is epidemic that affects an estimated one billion people worldwide. This nutrient is associated with many functions and organs in your body. Research shows that insufficient levels are associated with a greater rate of heart disease and mortality. Vitamin D levels less than 20 ng/mL are associated with a risk increase to 30 to 50 percent for developing colon, prostate, and breast cancer as well as an increased mortality from these cancers. In addition, vitamin D helps to maintain the health of your bones and muscles. The 22nd Annual National Association of Women Business Owner EPIC Awards dinner was held on Thursday, March 3, 2016, at 5:30 p.m. at the Mellwood Arts & Entertainment Center in Louisville, Kentucky. Louisville orthopedic surgeon and sports medicine doctor Stacie Grossfeld M.D. received the Small Business Owner of the Year Award.
The 22nd Annual National Association of Women Business Owner EPIC Awards dinner was held on Thursday, March 3, 2016, at 5:30 p.m. at the Mellwood Arts & Entertainment Center in Louisville, Kentucky. Louisville orthopedic surgeon and sports medicine doctor Stacie Grossfeld M.D. received the Small Business Owner of the Year Award. This special event, designed to recognize and celebrate the accomplishments of women business owners, included a cocktail reception compliments of Hilliard Lyons and a three-course dinner. Twelve award finalists gave brief speeches (complete with live voting from the audience) while Tim Laird, Chief Entertainment Officer of Brown-Forman Corporation, served as Master of Ceremonies, and Heather Howell, Director of Innovation at Brown-Forman, was the guest speaker.
This special event, designed to recognize and celebrate the accomplishments of women business owners, included a cocktail reception compliments of Hilliard Lyons and a three-course dinner. Twelve award finalists gave brief speeches (complete with live voting from the audience) while Tim Laird, Chief Entertainment Officer of Brown-Forman Corporation, served as Master of Ceremonies, and Heather Howell, Director of Innovation at Brown-Forman, was the guest speaker.
 Other 2016 EPIC Award recipients included Summer Auerbach, Owner of Rainbow Blossom, who received the Large Business Owner of the Year Award (for companies with more than 50 employees). EPIC stands for: Excellence as a woman business owner. Professional accomplishments during the past 5 years. Initiative and creativity in addressing major business challenges. Civic and community involvement.
Other 2016 EPIC Award recipients included Summer Auerbach, Owner of Rainbow Blossom, who received the Large Business Owner of the Year Award (for companies with more than 50 employees). EPIC stands for: Excellence as a woman business owner. Professional accomplishments during the past 5 years. Initiative and creativity in addressing major business challenges. Civic and community involvement.
 At some point in time, many people suffer from a broken wrist. Children and the elderly are at higher risk for this common injury. Follow along for more important information about symptoms and treatment options for a broken wrist.
At some point in time, many people suffer from a broken wrist. Children and the elderly are at higher risk for this common injury. Follow along for more important information about symptoms and treatment options for a broken wrist.
Recent Comments