
When it comes to concussions, oftentimes people are tricked into thinking that the symptoms and signs they experience are only temporary, since some of the more common ones aren’t necessarily considered severe. But this isn’t always true, and we’ll hear first-hand from Harriet Owen how brushing symptoms off, even after the smallest of head injuries, can be extremely detrimental in the scheme of recovery.
Concussion Symptoms, Signs, and Grades
This mild to severe system of recognition manifests in the existence of ‘grades’ that concussions can be classified by. While there is usually only one diagnosis of “yes, you have a concussion” or “no, you’re clear,” sometimes, a diagnosis can be furthered into 5 grades that build off of each other.
- Grade 0: A slight headache and perhaps some difficulty concentrating.
- Grade 1: A dazed or confused feeling for less than a minute.
- Grade 2: Cloudy, dazed, or confused senses that last longer than a minute, dizziness, amnesia, ringing in the ears, irritability
- Grade 3: Becoming unconscious for less than a minute
- Grade 4: Becoming unconscious for more than a minute
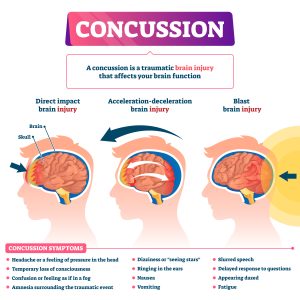
These aren’t the only symptoms of a concussion, though, and when it comes to the full list of signs of a concussion, the CDC categorizes them into 2 groups: observed and reported.
Observed symptoms are usually picked up externally, by outsiders who are watching the individual. This might include parents, teammates, coaches, friends, romantic partners, doctors, or trainers. It’s important to make note of head injuries so that if these signs do start appearing, then proper treatment can be sought and the injury isn’t left to become worse.
Observed Signs of Concussion:
- Can’t recall events prior to or after a hit or fall
- Appears dazed or stunned
- Forgets an instruction, is confused about an assignment or position, or is unsure of the game, score, or opponent
- Moves clumsily
- Answers questions slowly
- Loses consciousness (even briefly)
- Shows mood, behavior, or personality changes
Reported symptoms are the opposite – they usually don’t have any outward evidence (although some of them might), and it’s the individual that recognizes the change or feeling and then let’s someone else know.

Reported Signs of Concussion:
- Headache or “pressure” in head
- Nausea or vomiting
- Balance problems or dizziness, or double or blurry vision
- Bothered by light or noise
- Feeling sluggish, hazy, foggy, or groggy
- Confusion, or concentration or memory problems
- Just not “feeling right,” or “feeling down”
No matter how mild the concussion is, a checkup with a medical professional should be sought out, because brain injuries can be very dangerous, if given the chance.
Harriet Owen’s Growing Concussion Symptoms
Harriet’s specific symptoms provide a great example of what can happen if concussions are not taken seriously by individuals and the doctors that provide them care – what could have been a short recovery time snowballed into a 15 month period of pain, confusion, and misdirection.
Harriet describes the initial crash and subsequent signs as, “I knew almost immediately I’d hit my head, my helmet was scuffed and I had a bit of a headache, but I didn’t think it would have caused me a sustained concussion.”
This is why concussions are such slippery conditions – if it’s just a headache, it really doesn’t seem like anything to have to go to the doctor for. But even Grade 4 concussions can start out with symptoms of a Grade 0 concussion. Within a few days, that one small, unassuming headache didn’t go away and continued to become worse, and that’s when Harriet realized that something was wrong.
Her next problem? Her doctors didn’t. She was prescribed over the counter painkillers and more sleep, but no neurological or imaging tests were performed, even after persistent pain. Harriet began to experience more severe symptoms as time went on, with the reported worst being:
Even the smallest tasks drained her, and that led to more time inside, in dark rooms, and unable to do the things she loved. This contributed to the worsening of other symptoms such as depression and physical activity difficulties.
What started as a small symptom quickly turned unbearable. This led to light sensitivity and contributed to a lack of concentration and memory from the constant pain.
Without the ability to cycle and complete daily tasks without pain and other side effects, the pain combined with the fact that her brain couldn’t regulate her emotions as well as it had been caused personality changes in the form of depression, mood swings, and reactive behavior.
She says that, “…my change in personality really impacted everyone around me the most. I wasn’t myself; they didn’t know how I was going to react or be each day, and they didn’t know how to help me.”
- Lack of Concentration and Memory
Even as a professional cyclist, Harriet still has a full-time job as a data-analyst for Trek Bicycle Corporation, which involves a lot of screen time. The light from the screen triggered headaches and the work caused mental fatigue, even when she already felt that she couldn’t function at 100% due to her lack of concentration and memory, and that was demoralizing.
- Difficulties Participating in Physical Activity
Cycling is Harriet’s passion and her profession, so slowly becoming unable to ride at all became a dark spot in her life, and this big change in her life greatly affected her mental health.
She says, “Cycling for me during this time, was mostly non-existent or very inconsistent. If I ever did ride, it would be no longer than an hour at a lower heart rate, and my body would play catch-up, and I’d pay for it a couple of days later. It wasn’t healthy for me to keep being in this vicious cycle, so there was a long period of time that I just couldn’t ride. It affected me mentally, as well as physically, I lost a lot of muscle mass!”
When asked which symptoms impacted her daily life the most, Harriet quoted headaches, fatigue, and personality changes. But the shift from cycling every single day to barely being able to do an hour of low-heart rate exercises exacerbated her condition and the side effects that came along with it, and the initial habits she formed when she hadn’t gotten a concussion diagnosis ultimately hurt her recovery.
Concussions Are All Around

Especially in athletes, concussions are a likelihood of every head injury obtained. We’ve heard from a professional just how easy it is to brush off the burgeoning symptoms, and how that can play a part in the recovery process.
Even if you don’t encounter concussive accidents much in your sport, it’s still a big risk! As a cyclist, Harriet didn’t believe that concussions were all that common in cycling, but once she deliberated further, she realized that a cyclist hits their head more often than not when they crash their bike, which is just a part of the sport.
Helmets and other head safety gear provide some protection, but concussions occur internally. So, while your head might still be intact thanks to the helmet, your brain doesn’t have the same stability, and is very susceptible to injury and, subsequently, the side effects.
No element of a concussion is enjoyable, but the worst part, according to Harriet, is that, “Life as you know it is taken away from you the moment you hit your head. People can’t see the injury, so it’s hard to anyone to understand what you’re going through. It is a real mental battle to get back.”
What to Do If You Have a Concussion
Don’t let a concussion trip you up or slow you down! Get help and a diagnosis as soon as you recognize any sign or symptom of even a mild concussion. If caught early, no matter the grade, treatment and recovery time will be far less intense and the toll on your body far less severe.
In the third and final installment of this blog series, we’ll explore the extensive and innovative treatment that Harriet went through to get back to her best form, and what she might have done differently if she had known that she would end up with sustained concussion.
If you or someone you love has suffered a concussion or head injury in the Louisville, Kentucky area, board-certified sports medicine physician Dr. Stacie Grossfeld at Orthopaedic Specialists PLLC can help. Orthopaedic Specialists PLLC is accepting new patients, and same day appointments are available. For additional information or to schedule an appointment, please contact Orthopaedic Specialists PLLC today at 502-212-2663.






 There’s an age-old myth of ‘concussions don’t happen in non-contact activities’ that manages to fool many of us, but without proper gear, training, or awareness, you’re just as vulnerable to concussions in non-contact activities as you are in contact ones. And you can, of course, still get a concussion that isn’t sports-related – adults are especially prone to getting them as a result of a fall.
There’s an age-old myth of ‘concussions don’t happen in non-contact activities’ that manages to fool many of us, but without proper gear, training, or awareness, you’re just as vulnerable to concussions in non-contact activities as you are in contact ones. And you can, of course, still get a concussion that isn’t sports-related – adults are especially prone to getting them as a result of a fall. Having been cycling since she was 11 years old, Harriet Owen’s love for biking is a long, multi-generational one. Ever since she was a child growing up in Oxford, United Kingdom and watching her father compete in local races, Harriet looked at a bike and saw fun and excitement, but perhaps not her future as a professional cyclist, at the time.
Having been cycling since she was 11 years old, Harriet Owen’s love for biking is a long, multi-generational one. Ever since she was a child growing up in Oxford, United Kingdom and watching her father compete in local races, Harriet looked at a bike and saw fun and excitement, but perhaps not her future as a professional cyclist, at the time.



Recent Comments