Hand arthritis is a common condition that affects millions of people. The condition can cause pain, stiffness, and difficulty performing everyday activities that require movement in the hands. However, there are several types of hand arthritis, each with different causes and treatment options. Understanding the types of hand arthritis can help individuals find the best and most effective way to manage their condition. Every case is unique, but finding the origins of your pain is the first step towards treatment!
Types of Hand Arthritis
1. Osteoarthritis (OA)
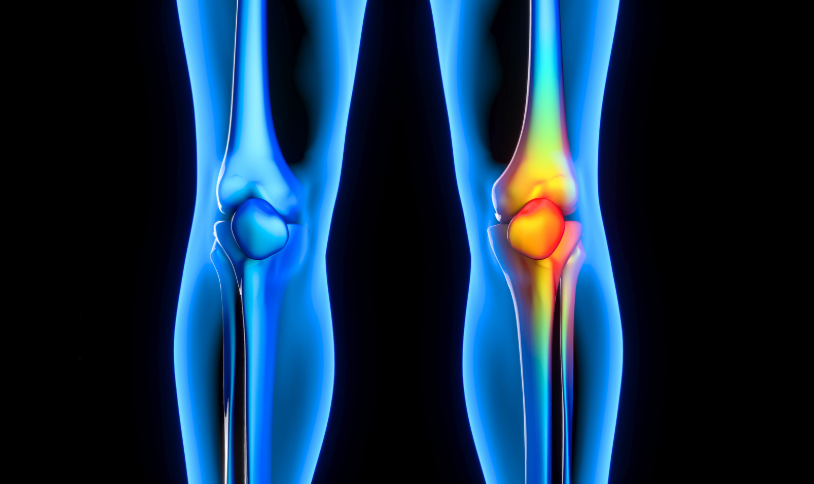
Osteoarthritis (OA) is the most common type of hand arthritis. It occurs when the cartilage that cushions the joints breaks down, which leads to pain, swelling, and limited mobility. OA is usually associated with age, but it can also occur due to genetics, previous injuries, or harsh, repetitive movements. In the early stages of OA, individuals may experience mild pain and stiffness, particularly in the morning or after periods of inactivity. As the condition progresses, there is a larger risk of joint deformities, swelling, and reduced range of motion.
Treatment for OA often focuses on relieving symptoms and maintaining joint function. Nonsteroidal anti-inflammatory drugs (NSAIDs), splints, and physical therapy can help manage pain and improve mobility. In more advanced cases, surgery, such as joint replacement or fusion, may be recommended.
2. Rheumatoid Arthritis (RA)
Rheumatoid arthritis (RA) is an autoimmune condition where the immune system mistakenly attacks healthy tissue, causing inflammation and damage in the joints. RA can affect both hands symmetrically, meaning it typically impacts the same joints on both sides of the body. RA commonly affects the wrist, knuckles, and the middle joints of the fingers and, if left untreated, can lead to joint deformities. The inflammation in RA can also affect the tendons and ligaments around the joints, which limits mobility and function even further.
Early diagnosis and treatment are key in managing RA. Disease-modifying antirheumatic drugs (DMARDs), biologics, and corticosteroid injections can help slow the progression of RA and reduce inflammation. Physical therapy is often recommended to maintain strength and mobility in the affected joints.
3. Post-Traumatic Arthritis
Post-traumatic arthritis (PTA) develops after an injury, such as a fracture or dislocation, damages the cartilage in the hand. Even if the injury heals properly, the cartilage may break down over time and result in joint pain and stiffness. Post-traumatic arthritis can develop years after the initial injury, especially if the trauma was severe or involved multiple fractures.
Symptoms of PTA include pain, swelling, and reduced range of motion in the affected joint. Treatment often involves managing pain with NSAIDs, using splints or braces to provide support, and engaging in physical therapy to strengthen the surrounding muscles. In severe cases, surgery may be required to repair damaged joints or replace them entirely.
4. Psoriatic Arthritis (PsA)
Psoriatic arthritis (PsA) is another autoimmune disease that affects the joints and is associated with the skin condition psoriasis. Psoriasis causes red, scaly patches to form on the skin, and individuals with PsA often experience joint pain and swelling in the hands, along with these skin patches. The hands may be affected by swelling, tenderness, and deformities in the fingers. PsA can also cause a condition known as dactylitis, which is characterized by swelling of the entire finger or toe.
The exact cause of PsA is unclear, but it is believed to be a combination of genetic and environmental factors. Treatment for PsA involves medications that control inflammation, such as NSAIDs, DMARDs, and biologics. Corticosteroid injections may also provide relief in certain cases.
5. Gout
Gout is a type of inflammatory arthritis caused by a buildup of uric acid crystals in the joints, which can form crystals that deposit in the joints. While gout most commonly affects the big toe, it can also affect the fingers and hands, causing sudden, intense pain, redness, and swelling. Gout attacks can happen unpredictably and may last for several days.
Risk factors for gout include obesity, excessive alcohol consumption, and a diet high in purines, which are found in red meat, shellfish, and alcohol. Treatment for gout includes medications to reduce pain and inflammation, such as NSAIDs, colchicine, or corticosteroids. Additionally, medications that lower uric acid levels, such as allopurinol, can help prevent future attacks.
If you or someone you love suffers from arthritis in the Louisville, Kentucky-area, board certified sports medicine physician Dr. Stacie Grossfeld at Orthopaedic Specialists PLLC can help. Orthopaedic Specialists PLLC is accepting new patients, and same day appointments are available. For additional information or to schedule an appointment, please contact Orthopaedic Specialists PLLC today at 502-212-2663.








Recent Comments