Meniscal Tear Surgery/Knee Scope/Knee Arthroscopy Overview
Orthopaedic Specialists 502-212-2663
Stacie Grossfeld, M.D. / Bess Fley, PA-C
Arrival to the Surgicenter Center
- You will be checked into the surgery center.
- Your vital signs, such as blood pressure and temperature, will be checked.
- A clean hospital gown will be provided.
- All jewelry, dentures, contact lenses, and nail polish must be removed or a very light color polish.
- An IV will be started to give you fluids and medication during and after the procedure.
- Your knee will be scrubbed and shaved in preparation for surgery.
- An anesthesia provider will discuss the type of anesthesia that will be used.
- Your surgeon will confirm and initial the correct surgical site.
Surgical Procedure
Meniscal Tear Surgery (Knee arthroscopy) is an outpatient procedure performed in a surgery center. The surgery itself takes Dr. Grossfeld approximately 20 minutes to complete. However, there is time needed to head back to the operating room, anesthesia needs to be administrated and positioning on the operating room table must occur. That will add total time to the meniscal repair procedure. After Dr. Grossfeld is complete with the surgical procedure there is time needed to wake up from the anesthesia and be transported back to the recovery room. When all the different components are added in the procedure is about one to 1.5 hours.
The knee arthroscopy is performed with a general anesthesia. You will be completely asleep for the surgery therefore you will not hear or see anything during the procedure.
Dr. Grossfeld will make three tiny incisions around the knee joint. The incisions are about a half inch in length.
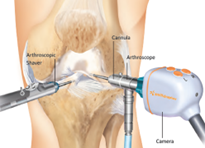 She will then insert a high-definition camera in the knee joint, which is about the size of a pencil. The internal part of the knee joint gets projected up onto a large 4K video monitor.
She will then insert a high-definition camera in the knee joint, which is about the size of a pencil. The internal part of the knee joint gets projected up onto a large 4K video monitor.
Dr. Grossfeld will inspect the whole knee joint. She will go through all three compartments of the knee. During this time she will assess for any damage and/or pathology that needs to be fixed surgically. Dr Grossfeld will also document abnormal findings if any. Color photos are taken throughout the procedure.
While performing the knee arthroscopy, Dr. Grossfeld, will identify the meniscal tear(s), and or any other pathology. She will remove the part of the meniscus that is torn with a pair of microscopic scissors and buff the edges. If the meniscus is a repairable-type tear (very rare <2% of meniscal tears are repairable), then a series of sutures (stitches) will be placed in the meniscus to repair it.
When the torn part of the menisci is removed, the remaining portions of the meniscus, that is healthy, remains in the knee joint. The remaining meniscus will function as a shock absorber for the knee joint.
When the meniscus is torn, it is very painful, and by removing the torn portion of the meniscus, the pain goes away.
At the end of the surgical procedure, Dr. Grossfeld will inject numbing medicine into the incision sites so there is typically very little pain immediately post-surgery. Most people will use less than three pain pills, and many times your pain is controlled with just ibuprofen and/or ice along with Tylenol.
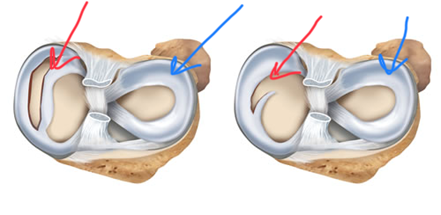
The images above: the red arrows reveal the torn meniscus. The blue arrows show a normal meniscus. The image to the left is a bucket handle meniscal tear and the image on the right: a radial type meniscal tear.
There will be no sutures placed in the incision sites. Dr. Grossfeld will use little white Band-Aids called Steri-Strips to close the portal sites. Therefore, there are no sutures that will need to be removed post operatively. It is completely normal to bleed through the dressings and for the steri-strips to have dried blood on them once the dressing is removed. Please leave the steri-strips on until your first post operative visit. They are closing the surgical incisions and the incision site will need about 7-9 days to heal. If the steri-strips fall off on their own that is okay.
Surgical Dressing
At the end of the surgery, Dr. Grossfeld, will put on a dressing. The dressing is a bunch of 4×4 gauze pads, an abd pad, followed by cast padding (stretchy white material). An Ace Wrap is then placed around the knee on top of the dressings listed above. The ace wrap can be discontinued when the swelling in the knee joint is minimal. The ace wrap helps to reduce swelling. Dr Grossfeld recommends wearing the ace if there is swelling present. Please refer to your post operative orders that you will receive day of your meniscal tear surgery for dressing change details.
Dressing to purchase before your surgery day are: ten 4×4 gauze pads, an extra 6-inch ace wrap, and peroxide.
Recovery Room
After surgery, you will be transported to the recovery room for close observation of your vital signs and circulation. You may remain in the recovery room for one to two hours depending on how quick you recover from the anesthesia.
Crutches
Crutches may or maybe not be used or needed. Crutches will be supplied by most surgery centers. Amazon also sells different types of crutches. Most people are off crutches within 2-4 days of the meniscal tear surgery. Some patients do not even use crutches but that is patient dependent.
Post Operative Care of the Knee: Ice/Showering
 You will be provided with a detailed set of instructions on how to take care of your knee after meniscal tear surgery.
You will be provided with a detailed set of instructions on how to take care of your knee after meniscal tear surgery.
It is very important to use ice as MUCH as possible. Dr. Grossfeld orders continuous use of ice around the clock. The rule is you cannot use too much ice. Berg Polar Care Unit can be purchased from our office.
We recommend using it continuously for 3-4 days after surgery. We recommend that you sleep with the Berg Polar Care Unit around the knee joint so ice is being applied all night. It is the best source of pain control and helps to reduce swelling.
The Berg Polar Care unit is filled with ice and water. It has a hose that connects to a neoprene wrap that goes around the knee, and will push ice water through the neoprene wrap for up to nine hours. The unit is motorized and plugs into an electrical socket. We actually recommend you use ice around the clock. We recommend that you sleep with ice around the knee. It is the best source of pain control and helps to reduce swelling. The Berg Polar Care Unit can be purchased from Dr. Grossfeld’s office. Ask any of the assistants.
The first couple of days after surgery plan on limiting your activity and keeping your leg elevated above your heart to reduce swelling. Work on moving your foot up and down to prevent blood clots in the lower leg.
It is normal to have swelling in the ankle, foot, and toes after surgery. What is not normal is if there is pain in the calf area of the lower leg. That can be a sign of a blood clot. If that occurs a visit to the emergency department is needed immediately.
You will be given detailed instructions on how to do the dressing changes after surgery. The post operative orders will be given to you the day of surgery. Make sure you read them.
Keep the knee dry. You can shower but put a water proof wrap around the knee such as a garbage bag or Saran Wrap. You may shower right away as long as the knee stays dry.
Night of Surgery
Anesthesia will recommend that you have a family member or friend stay with you over night for the first night after surgery. Ice is your best friend. Take your pain meds or anti-inflammatory medication before you go to bed and first thing the next morning.
Pump your feet and ankles up and down to help prevent blood clots from forming in the legs. Once you start walking; pumping the foot and ankles becomes less necessary.
Post-Surgery Activity
Full weight-bearing is allowed, for most patients. Your postop instructions will detail weight bearing status. Climbing stairs is okay if you feel comfortable and do not feel like you will lose your balance. If your bedroom is upstairs and you are worried about stability, it is okay to scoot up the stairs on your bottom.
Please start to work on range of motion exercises for the knee to help prevent excessive stiffness and this will also help to reduce swelling.
Most people are driving within a week.
Follow-Up
You will follow up postoperatively in the office, approximately 10-14 days after surgery.
Physical therapy may be recommended based on range of motion and function of your knee. The need for physical therapy is determined at this appointment. The majority of patients do not need physical therapy after a knee arthroscopy.
Return to Work
Each person’s job description, and pain level is unique, therefore, the return-to-work capability is made on a patient-by-patient basis.
However, in general, if you have a labor type position, then return-to-work capability is typically within 4-6 weeks after surgery. If your employment is a sit-down type job, then return-to-work capability can be either before the first week postoperative or just shortly after the first postoperative appointment. Return to work is very individualized. Dr. Grossfeld will involve you in the decision to work and what restrictions may be needed.
Finally, it is important to keep in mind, if arthritis is found in the knee joint at the time of the surgical procedure, it may get flared up from the surgery. If that occurs it may necessitate that a cortisone injection be given a couple weeks post-surgery.
FMLA and Disability Paperwork
Our office offers the service of completing paperwork for FMLA and/or disability for a fee of $40, per set of paperwork, and is completed in the order that it is received, typically takes 7-10 business days. All requests must originate with your employer, as your eligibility for FMLA and/or disability is based on your benefits with your employer. While each patient is unique, we do our best to estimate the time of recovery and often over-estimate the amount of time to prevent a lapse in benefits and/or require additional paperwork. Often disability companies require updates after each appointment. It is the patient’s responsibility to communicate this request with the office. Updates are not automatically completed. Any questions regarding this can be directed to Dorothy.

Recent Comments