
Key Takeaways:
- Osteoarthritis is an active, or progressive, disease that gets worse with time and cannot be cured.
- Osteoporosis is a curable disease.
- To treat osteoporosis, patients will use a combination of additional vitamins, weight-bearing exercises, and prescription medication in some cases.
Osteoporosis and osteoarthritis are two conditions that patients may get mixed-up about. Both are having to do with the bones, as denoted by the shared “osteo-” prefix. However, these conditions are very different from each other. One of the biggest differences is that one is curable, and one is not.
Progressive vs Non-Progressive Conditions
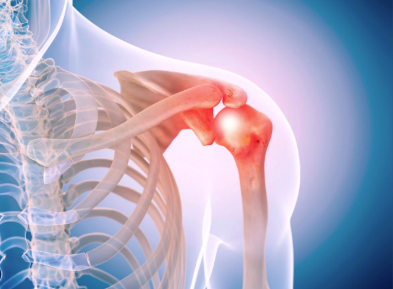
When a condition is progressive, it means that you cannot reverse or cure it. Osteoarthritis, which is when the cartilage around the joints and ends of bones wears away, is one of these conditions. Because it cannot be reversed, treatment focuses on slowing the progression of the condition and managing symptoms instead of eliminating them altogether.
On the other hand, non-progressive conditions are reversable. Osteoporosis, or the softening of the bones, is an example of a non-progressive condition, despite the fact that the symptoms can worsen if the condition is left untreated.
What are the Symptoms, Treatments, and Risk Factors for Osteoarthritis?
Osteoarthritis usually presents symptoms in the knees, hips, hands, and spine. These can include:
- Joint pain that worsens with activity
- Stiffness (especially in the morning or after inactivity)
- Swelling around the joint
- Reduced flexibility and range of motion
- Grinding or clicking sensation
- Bone spurs in advanced stages
Since it is a progressive disease, treatment focuses on managing symptoms, not curing osteoarthritis. Most of these methods are non-medicinal lifestyle changes like losing weight, implementing weight-bearing exercises into your routine, and monitoring your diet for inflammatory trigger foods.
Factors that increase the risk of osteoarthritis are:
- Age
- Hormonal shifts like menopause
- Obesity
- Joint Injuries
- Genetics
- Repeated joint stress
- Sex assigned at birth
What are the Symptoms, Treatments, and Risk Factors for Osteoporosis?
Osteoporosis is a silent disease, meaning that it doesn’t show many symptoms. In the case of osteoporosis, many people don’t know that they have the condition until they experience a break or fracture due to brittle bones, most commonly in the hips, wrist, or spine. However, other symptoms may include:
- Back pain
- Loss of height
- Stooped posture, also known as kyphosis
Treatment of osteoporosis focuses on strengthening bones, muscles, and slowing bone loss. Focusing on a diet rich in vitamin D and calcium, as well as implementing weight-bearing exercises, strength training, and balance training to reduce fall risks into routines are common treatments. Medication could be used in some cases. Regular DEXA scans, or bone density tests, are usually also recommended to track progress and risk.
Factors that increase the risk of osteoporosis are (Northwell Phelps Hospital):
- Age
- Sex assigned at birth
- Genetics
- Hormonal shifts like menopause
- Ethnicity (White or Asian Descent)
- Smoking
- Alcohol use
- Sedentary lifestyle
- Pre-existing medical conditions
If you or someone you love suffers from a bone-related condition like osteoarthritis or osteoporosis in the Louisville, Kentucky-area, board certified sports medicine physician Dr. Stacie Grossfeld at Orthopaedic Specialists PLLC can help. Orthopaedic Specialists PLLC is accepting new patients, and same day appointments are available. For additional information or to schedule an appointment, please contact Orthopaedic Specialists PLLC today at 502-212-2663.








Recent Comments