
It’s no secret that knees are an incredibly vital, yet vulnerable joint in our bodies. From supporting our weight to the ability to walk, having healthy, mobile knees is crucial to activity and our comfort when we move our bodies into different positions on different surfaces. When we were children, perhaps it was easy to get into certain positions that you have difficulties achieving as an adult, a very common position being sitting cross-legged. If this position causes you discomfort or pain, then you might be wondering what could be wrong with your your knee to suddenly have that pain.
Having knee pain in any position might be alarming, and it’s important to get to the bottom of your knee pain before it worsens. Here’s 6 different reasons that your knee hurts when your sit cross-legged!
1. A Previous Injury
It can be frustrating when we get injured, but it can be even more frustrating when we think that our bodies are healed and then start experiencing pain again. The knee is a very vulnerable part of our body, as it is a joint that is under a lot of repetitive pressure during most of our day. In a study from the Osteoarthritis Initiative, experts saw a 3-6x increase in the likelihood of osteoarthritis and earlier onset of symptoms in individuals with a prior knee injury. Young athletes are also more than 5x more likely to experience an ACL tear in either knee when they have already torn their ACL.
Some of this risk and lingering pain can be offset by preventative measures taken in the recovery period, such as rigorous physical therapy, personal training to strengthen the area, and keeping away from physical activity until the knee injury is completely healed instead of pre-maturely putting the joint back to work that it isn’t ready for.
2. Weakened Hips or Glutes
A sedentary lifestyle can lead to the weakening of the gluteal and hip muscles, which means that when weight is loaded onto the legs, those muscles cannot preform optimally and forces other areas of the body to compensate – the knees being one of the first to face the consequences. This weakening can also lessen the body’s ability to absorb shock and move correctly, which leads to awkward movements becoming habit and excess strain wearing down joints.
3. Arthritis
Sometimes, knee pain is due to the normal wear-and-tear of our aging bodies. Osteoarthritis and Rheumatoid Arthritis are both conditions that affect more than 32 million adults in the US. The symptoms include pain, stiffness, and loss of joint movement. Arthritis causes the cushioning cartilage of the knee joint to wear away until the bones rub together directly; this can affect the outer compartment of the knee (lateral knee pain), the inside compartment (medial knee pain), and underneath the knee cap (patellofemoral knee pain).
4. Runner’s Knee
A common cause of knee pain when bent into a certain position is overuse of the muscles and joint. Runner’s knee is the term that describes patellofemoral pain and occurs mostly in runners, hikers, skiers, cyclists, soccer players, weightlifters, and women in general, as their proportions make it easier for the knees to be worked at an unnatural angle. There can be a popping or cracking noise with knee flexion, but can be improved with rest, physical therapy, and knee support.
5. Tendonitis
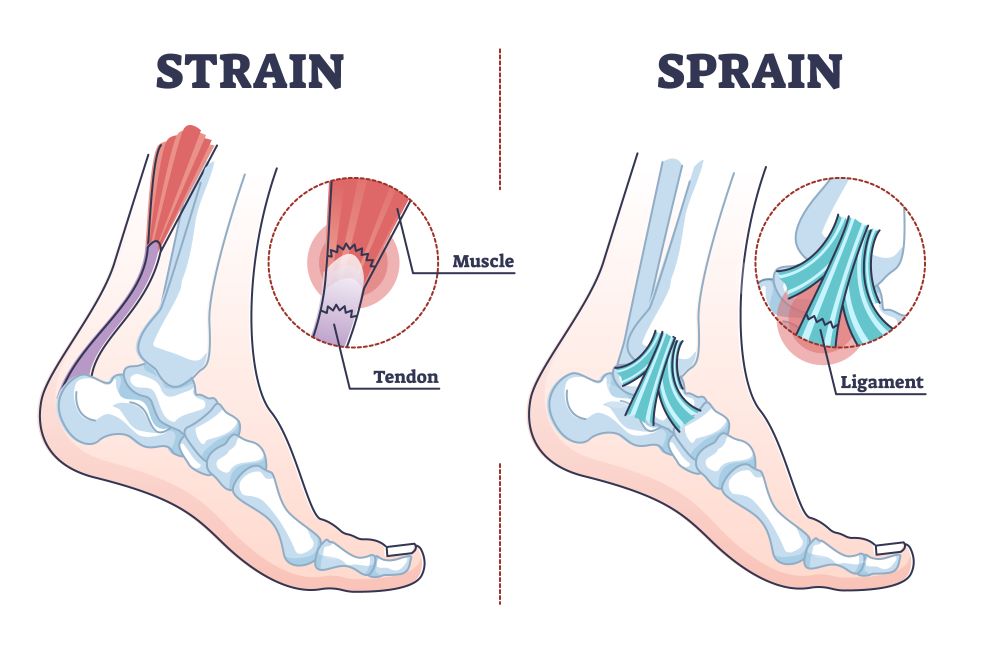
Tendonitis, or the inflammation of tendons, can affect knee pain because the knee is surrounded and supported by a myriad of tendons from the back of the thigh and knee (hamstring tendonitis), the front of the knee (patellar tendonitis), and above the knee (quadriceps tendonitis). Tendonitis pain is triggered by bending and movement of the knee, which is required in order to be able to sit cross-legged.
6. Iliotibial Band Syndrome (ITBS)
Outside of the knee pain is often caused by outside of the knee anatomy, and the iliotibial band is a prime suspect as a thick strip of connective tissue from the outer hip to the shin. Iliotibial Band Syndrome (ITBS) is most common in male athletes but can affect anyone of any gender who engage in repetitive motion using the Iliotibial band. This overuse causes the tightening and/or inflammation of the IB, and the irritation can spread to nearby tissue as well, both of which you would feel when sitting cross-legged.
If you or someone you love has suffered a knee injury in the Louisville, Kentucky-area, board certified sports medicine physician Dr. Stacie Grossfeld at Orthopaedic Specialists PLLC can help. Orthopaedic Specialists PLLC is accepting new patients, and same day appointments are available. For additional information or to schedule an appointment, please contact Orthopaedic Specialists PLLC today at 502-212-2663.

 For many of us that lead busy lives, there never seems to be much time to commit to the proper amount of exercise recommended, which is 30-60 minutes per day for adults. Between managing a family, having a full-time job, cooking healthy meals, and taking care of our home and other responsibilities, getting a gym membership on top of it all seems like a moot point. But there are plenty of easy exercises to strengthen your joints and muscles that you can get from the comfort of your home, or even during your day by making conscious choices; a popular one? Walking!
For many of us that lead busy lives, there never seems to be much time to commit to the proper amount of exercise recommended, which is 30-60 minutes per day for adults. Between managing a family, having a full-time job, cooking healthy meals, and taking care of our home and other responsibilities, getting a gym membership on top of it all seems like a moot point. But there are plenty of easy exercises to strengthen your joints and muscles that you can get from the comfort of your home, or even during your day by making conscious choices; a popular one? Walking!

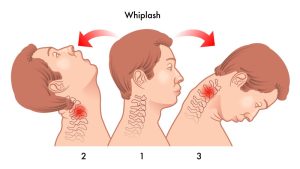 This type of injury is known by terms other than whiplash, such as neck strain or neck sprain, so it might be called by a different name when it comes to articles on the internet or health providers. It also refers to a broader range of injuries rather than just one, like most other injury-related terms do, because when the neck bounces back and forth, the muscles, ligaments and tendons, and/or joints are manipulated past the point of their normal range of motion.
This type of injury is known by terms other than whiplash, such as neck strain or neck sprain, so it might be called by a different name when it comes to articles on the internet or health providers. It also refers to a broader range of injuries rather than just one, like most other injury-related terms do, because when the neck bounces back and forth, the muscles, ligaments and tendons, and/or joints are manipulated past the point of their normal range of motion.



Recent Comments