
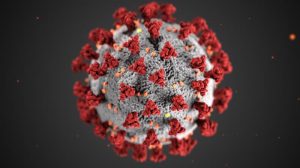
Keeping active during the pandemic is important for your health and wellness. It can be hard to evaluate what the level of risk is with different activities, though. You may have questions like: when do I need to wear a mask, what should I avoid doing, and is it safe to go to a gym? Let’s take a look at the facts to help you make the best decisions as you stay active.
General Considerations During the Pandemic
As with many decisions in the pandemic, a lot of your choices will have to be in context locally. Where you are has a huge impact on what sorts of activities are more or less safe. So, for starters, make sure you follow your state and local-level guidelines. If certain activities are temporarily halted, like going to a gym or gathering with a group to work out outside, heed the advice of your public health officials. If there’s a lot of disease spread in your area, you should be a bit more careful than if community transmission is largely under control where you live.
Additionally, you should take your own risk level into account when deciding between different activities. For one thing, the risk of severe illness from the coronavirus increases with age. A 70 year old is at a higher risk for severe illness than a 20 year old. Additionally, any existing medical conditions may increase your risk. There are several conditions that increase risk, from heart conditions to cancer and obesity. See the CDC’s guidelines here for more information.
With all of that in mind, you can start to think through your options. Now let’s take a look at some of the risks associated with different types of activity.
Outside Activities
In general, we know that interactions outside are much safer than those inside relative to coronavirus spread. Still, it’s important to think through how close you may need to get to other people outside during exercise. If you are running, walking, or cycling by yourself or with a small trusted group, that’s relatively low risk. However, a crowded walking path or park may be a higher risk if you have to be close to other people.
Plus, if you are going to exercise with others, there is a level of risk associated if you get too close with them. Depending on the activity, you may be able to distance or wear a mask to mitigate risk. Keeping any group sizes as small as possible, distancing, only exercising with people you trust, and masking if needed can all help you keep yourself and others safe.
Indoor Activities
Being inside with others is higher risk compared to outside during the pandemic. In many places, indoor spaces like gyms and studios have reopened with many precautions in place. You should consider the layout and precautions for the space you may exercise in. For example, some fitness businesses have been able to keep windows open, increase airflow, enforce good distancing, and require mask-wearing. If these precautions are in place, they create a safer space for exercising.
To conclude, any decision you make about exercising around others is very contextual during the pandemic. Your own risk factors, disease spread in your community, and the specifics of where and how you will be exercising around others all come into play. There is no one size fits all answer here- just make sure you take everything into account as you decide what’s best for you.
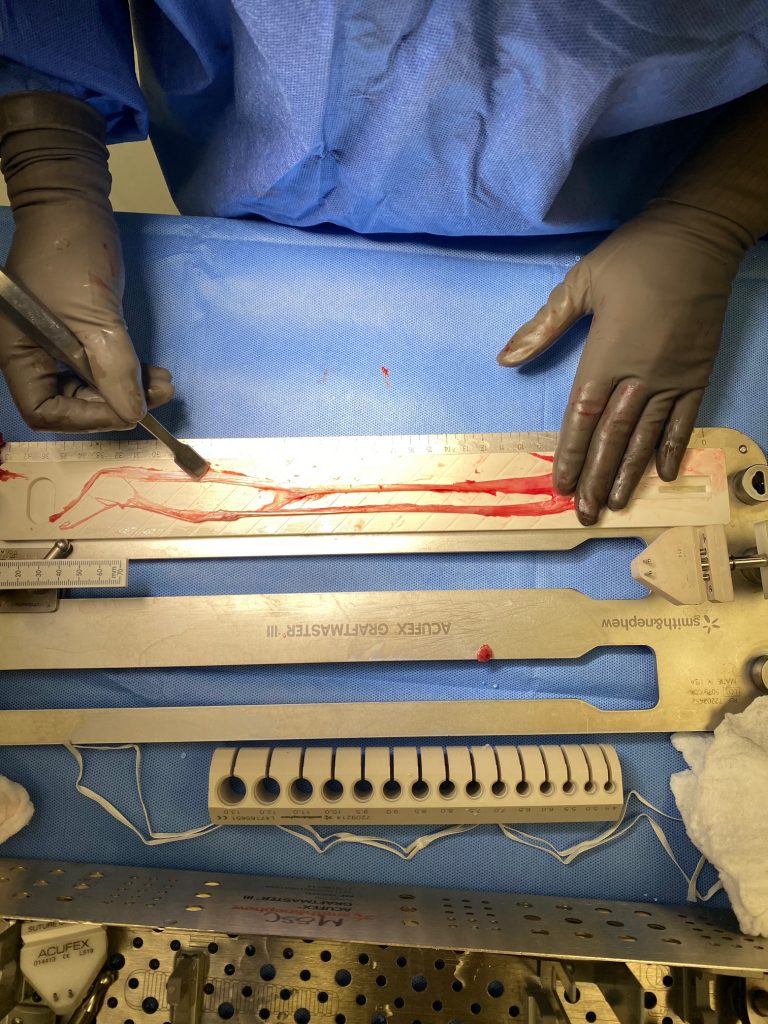
You should seek diagnosis and treatment from a qualified medical professional like Dr. Stacie Grossfeld if you are injured and want to get back to the activities you love. To schedule an appointment with Dr. Grossfeld, call Orthopaedic Specialists at 502-212-2663 today.










Recent Comments