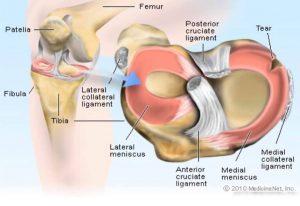
1. Sharp, stabbing pain located in your knee joint.
2. It is easy to localize the pain in the knee and it is consistently in the same place.
3. No pain occurs when resting. Pain occurs with a plant and a twist, lateral motion or flexion of the knee.
4. Slight swelling is present and the knee can feel tight with a slight limit of motion.
5. Clicking, locking of the knee and popping may occur.











Recent Comments