 Carpal tunnel syndrome is a common condition that causes numbness, tingling, weakness, and other discomforts in your hands and fingers. A pinched median nerve in your wrist causes these discomforts. The median nerve, along with other related tendons, travels from your forearm to your hand inside a small space called the carpal tunnel. This nerve supplies feeling and movement to your thumb as well as your first three fingers. When the median nerve is under pressure or becomes pinched, it is called carpal tunnel syndrome.
Carpal tunnel syndrome is a common condition that causes numbness, tingling, weakness, and other discomforts in your hands and fingers. A pinched median nerve in your wrist causes these discomforts. The median nerve, along with other related tendons, travels from your forearm to your hand inside a small space called the carpal tunnel. This nerve supplies feeling and movement to your thumb as well as your first three fingers. When the median nerve is under pressure or becomes pinched, it is called carpal tunnel syndrome.
Carpel tunnel syndrome is the most common type of entrapment neuropathy and is sometimes confused with other illnesses such as hypothyroidism, rheumatoid arthritis, and diabetes. Repetitive movements, such as typing, texting, using a computer mouse, and oddly enough, even pregnancy, can cause some common carpal tunnel symptoms. These include things like swelling, tingling, and numbness in the thumb, index finger, middle finger, and half of the ring finger. If you are experiencing these symptoms in your little (or pinky) finger then this is a good indicator that your symptoms are not related to carpal tunnel syndrome.
Carpal tunnel symptoms can be confused with other medical conditions or illnesses, so consult a qualified medical doctor for a complete examination. Read 10 carpal tunnel symptoms as detailed by board certified orthopedic surgeon and sports medicine physician Dr. Stacie Grossfeld.
10 Symptoms of Carpal Tunnel Syndrome You Should Know
Numbness
This is the first indicator that something may be wrong. Pressure on the median nerve causes numbness or tingling in your hand and fingers. Usually the numbness related to carpal tunnel will wake you up in the middle of the night.
Tingling
Like numbness, carpal tunnel can cause a “pins and needles” feeling to your hand and fingers.
Pain
Carpal tunnel can be somewhat painful, making repetitive movements more difficult.
Stiffness
Usually people with carpal tunnel will experience stiffness in the hands, fingers, and wrist. This stiffness is usually more severe in the morning.
Weakness
The compression in your wrist, hands, and fingers may cause weakness. Carpel tunnel syndrome often makes holding objects or writing more difficult.
Elbow Pain
It is not uncommon for people with carpal tunnel syndrome to have pain or tingling in the elbow.
Difficulty Falling Asleep
Carpal tunnel syndrome causes tingling and pain which distracts the mind and makes it harder to fall asleep. The constant pins and needles feeling may make it difficult for you to relax and get a good night’s sleep.
Pain in One Hand More than the Other
Generally people with carpal tunnel will experience more severe symptoms in one hand than the other. This is due to repetitive movements and left or right hand dominance.
Shoulder Pain
Many people with carpal tunnel syndrome have even experienced pain, tingling, or numbness running all the way from their shoulder down to their fingertips. Where you feel pain completely depends on where the pressure on your nerve is located.
Decrease in Grip Strength
Along with weakness in hand and finger muscles, carpal tunnel syndrome may make it difficult for you to hold relatively easy to grasp objects and open containers.
Carpal tunnel symptoms can be unnerving, pun intended! If you are experiencing any of these symptoms regularly and if everyday activities are becoming difficult, it is worth a visit to your doctor’s office. A thorough physical exam will identify carpal tunnel syndrome.
Most of the time home treatment options for carpal tunnel syndrome are successful. Change activities that are causing pain along with physical therapy. You may also be prescribed nonsteroidal anti-inflammatory drugs to reduce inflammation. If your condition worsens, surgery may become an option.
It is best to treat this early before any carpal tunnel symptoms lead to long-term effects. For more information about this condition or to schedule an appointment in Louisville, Kentucky, with a board certified orthopedic surgeon, call Dr. Grossfeld’s office at 502-212-2663.

 Dr. Grossfeld was privileged enough to be invited to the Bingham Fellows Program Class of 2016 graduation at Actor’s Theater in the Victor Jory Theatre. Dr. Grossfeld serves on the Board of both the Louisville Sports Commission and the YMCA at Norton Commons, and the CEO and President of both organizations were a part of the 2016 graduating class. Dr. Grossfeld elaborates:
Dr. Grossfeld was privileged enough to be invited to the Bingham Fellows Program Class of 2016 graduation at Actor’s Theater in the Victor Jory Theatre. Dr. Grossfeld serves on the Board of both the Louisville Sports Commission and the YMCA at Norton Commons, and the CEO and President of both organizations were a part of the 2016 graduating class. Dr. Grossfeld elaborates: Metro Specialty Surgery Center in Louisville, Kentucky is having a pumpkin decorating contest and guess who’s face they chose to decorate as a pumpkin? Dr. Grossfeld!
Metro Specialty Surgery Center in Louisville, Kentucky is having a pumpkin decorating contest and guess who’s face they chose to decorate as a pumpkin? Dr. Grossfeld!
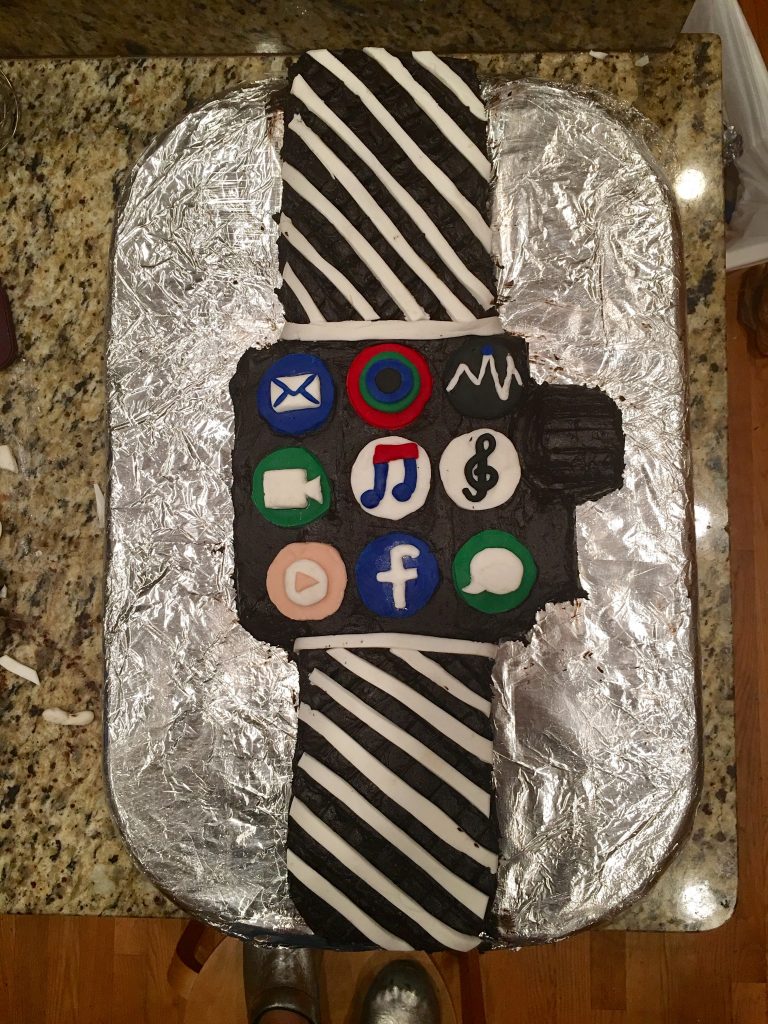 Talking about baking the Apple Watch birthday cake, Dr. Grossfeld explains that she really only bakes once a year outside of an occasional batch of cookies and apple or cherry pie.
Talking about baking the Apple Watch birthday cake, Dr. Grossfeld explains that she really only bakes once a year outside of an occasional batch of cookies and apple or cherry pie.




 For many people living in tropical regions in Central and South America, the Zika virus has been a concern since the 1950s. Recently, the Zika virus has spread at an alarming rate. And now the virus has traveled to North America with 14 known cases in Miami, Florida in August 2016. This virus is extremely worrisome for pregnant women or those looking to become pregnant. The Zika virus causes serious birth defects in children born to a Zika infected woman.
For many people living in tropical regions in Central and South America, the Zika virus has been a concern since the 1950s. Recently, the Zika virus has spread at an alarming rate. And now the virus has traveled to North America with 14 known cases in Miami, Florida in August 2016. This virus is extremely worrisome for pregnant women or those looking to become pregnant. The Zika virus causes serious birth defects in children born to a Zika infected woman.
Recent Comments