Dr. Grossfeld Hosts Social Event for Juniors Competing in 2016 USA Cycling Amateur Road Nationals in Louisville
 The 2016 USA Cycling Amateur Road Nationals is taking place in Louisville, Kentucky, June 30, 2016 through July 3, 2016. Kids from all over the United States are in Louisville to participate in this annual event. The 2016 USA Cycling Amateur Road Nationals includes a criterium, road racing, time trials and a national championship. This cycling event is sponsored by Papa John’s.
The 2016 USA Cycling Amateur Road Nationals is taking place in Louisville, Kentucky, June 30, 2016 through July 3, 2016. Kids from all over the United States are in Louisville to participate in this annual event. The 2016 USA Cycling Amateur Road Nationals includes a criterium, road racing, time trials and a national championship. This cycling event is sponsored by Papa John’s.
In order to bring together kids from across the country, Louisville orthopedic and sports medicine doctor Stacie Grossfeld decided to kick off the event by hosting a special celebration at her home on Tuesday, June 29, 2016. The  event included 90 youth cyclists representing top teams from all over the USA. Louisville-area youth in attendance included cyclists from the: Papa John’s Racing Team, Revolution Devo Cycling, Better Cycling of Louisville, Team Louisville, and TWENTY16.
event included 90 youth cyclists representing top teams from all over the USA. Louisville-area youth in attendance included cyclists from the: Papa John’s Racing Team, Revolution Devo Cycling, Better Cycling of Louisville, Team Louisville, and TWENTY16.
This special social event gave the kids participating in the 2016 USA Cycling Amateur Road Nationals the rare opportunity just to relax, socialize and get to know other cyclists and coaches from across the country.
Describing the event, Dr. Grossfeld explained: “In the
beginning, the kids were hanging out in small groups with their team members but after a little while, it was great to see that kids from all the teams were socializing together, playing tennis, basketball, swimming, eating, and just having a good time.”
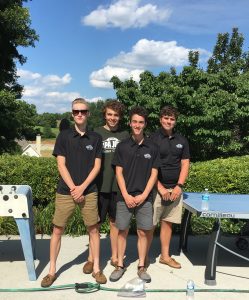
Cyclists on the Papa John’s Youth Cycling Team enjoy socializing before the kick off of the 2016 USA Cycling Amateur Road Nationals.
During the event, attendees enjoyed playing basketball, swimming, playing tennis, sharing stories, and eating….(and eating and eating). In fact, Dr. Grossfeld noted that this healthy, fit and active group of kids managed to eat over 100 hamburgers and buns, 30 pounds of fruit salad, 18 pounds of tortellini, 10 pounds of veggie trays , 3 mega bags of chips , 2 pounds of hummus, half pound of pesto, 10 pounds of french fries and 120 cookies!!! (more…)


 level, is earning and cementing the trust of the athlete. “Loyalty is earned in this field and can be very temperamental,” Dr. Cole said. He noted that in the national football league, it was reported recently that a significant percentage players distrusted their team physician.
level, is earning and cementing the trust of the athlete. “Loyalty is earned in this field and can be very temperamental,” Dr. Cole said. He noted that in the national football league, it was reported recently that a significant percentage players distrusted their team physician. Remember that the most common way to sustain an ACL injury occurs through non-contact situations, such as the basketball player dribbling the ball down the court, stopped quickly, and tears his ACL. This is similar to the soccer player who is running down the field and she stops and pivots quickly and tears her ACL. A contact ACL injury occurs when there was actually contact from another player to the injured athlete’s knee, which is less common that the previous examples.
Remember that the most common way to sustain an ACL injury occurs through non-contact situations, such as the basketball player dribbling the ball down the court, stopped quickly, and tears his ACL. This is similar to the soccer player who is running down the field and she stops and pivots quickly and tears her ACL. A contact ACL injury occurs when there was actually contact from another player to the injured athlete’s knee, which is less common that the previous examples. Athletes are not the only one’s susceptible to this type of injury, but their level of activity and repetitive movements put athletes at a higher rate of risk for sustaining this injury. Fortunately there
Athletes are not the only one’s susceptible to this type of injury, but their level of activity and repetitive movements put athletes at a higher rate of risk for sustaining this injury. Fortunately there involve a lot of jumping can be prone to developing stress fractures. Also, those with osteoarthritis often developed stress fractures due to their weakened bones.
involve a lot of jumping can be prone to developing stress fractures. Also, those with osteoarthritis often developed stress fractures due to their weakened bones.
 every case is specific for each athlete and injury, new information about ACL reconstruction surgery has been published to provide a better insight into this type of injury.
every case is specific for each athlete and injury, new information about ACL reconstruction surgery has been published to provide a better insight into this type of injury. 7.8 per 1000 male patients. The second highest incidents were among those ages 50 to 59 years of age, where the distribution of male and the female patients was equal.
7.8 per 1000 male patients. The second highest incidents were among those ages 50 to 59 years of age, where the distribution of male and the female patients was equal. The Orthopaedic Specialists’ management team, including Dr. Stacie Grossfeld (orthopedic medical practice owner) Tisha Robison (orthopedic medical practice manager) and Dorothy Cochran (assistant practice manager)) enjoyed participating in a workshop for Louisville, KY-area businesswomen sponsored by PNC and held at the PNC tower downtown. A presentation by
The Orthopaedic Specialists’ management team, including Dr. Stacie Grossfeld (orthopedic medical practice owner) Tisha Robison (orthopedic medical practice manager) and Dorothy Cochran (assistant practice manager)) enjoyed participating in a workshop for Louisville, KY-area businesswomen sponsored by PNC and held at the PNC tower downtown. A presentation by  Operating Officer of HDTV. Under Packard’s leadership, HDTV became one of the fastest-growing cable networks in TV history. Packard help build Scripps Networks Interactive into a market value worth over $10 billion. Now Susan works as a writer, speaker and consultant to business women in every stage of life. She serves as mentor and guide, helping women learn how to achieve success at home and at work.
Operating Officer of HDTV. Under Packard’s leadership, HDTV became one of the fastest-growing cable networks in TV history. Packard help build Scripps Networks Interactive into a market value worth over $10 billion. Now Susan works as a writer, speaker and consultant to business women in every stage of life. She serves as mentor and guide, helping women learn how to achieve success at home and at work.
Recent Comments