
In 1971, before Title IX had past, it was estimated that 310,000 female athletes were participating in 
sports. In 2010 there were approximately 3,373,000 female participants. Over this period of time, a phenomenon described as the Female Athlete Triad has become an increasing concern for female athletes.
An excellent review article was published regarding the female athlete triad: past, present, and future in the July, 2015 issue of the Journal of the American Academy of Orthopedic Surgeons. The article was written by Dr. Elizabeth Matzkin, Emily Curry, and Kaitlyn Whitlock, PA – C. Highlights of the article are covered below.
In 1992, the task force on women’s issues of the American College of sports medicine was assembled, and the term “female athlete triad” was created to define the three components that characterize this condition. The definition of the female athlete triad, at that time, had to include disordered eating, osteoporosis, and amenorrhea.
 It was noted that the athletes that appeared to be at highest at risk were the ones involved in endurance sports that emphasize low body weight, and athletes that were involved in sports that included subjective judging such as figure skating and gymnastics.
It was noted that the athletes that appeared to be at highest at risk were the ones involved in endurance sports that emphasize low body weight, and athletes that were involved in sports that included subjective judging such as figure skating and gymnastics.
For prevention, diagnosis and treatment of this condition it is very important that people involved with the athletes are aware of the diagnosis. This includes coaches, team physicians, parents, colleagues, and teammates. In 2006 there was a survey of Division I college coaches. Sixty-four percent of 91 respondents were aware that the female athlete triad existed, but only 43% were able to appropriately identify the three components. In a separate study of physicians, physical therapists, coaches and athletic trainers, less than half were able to name the three components of the triad, with only 40% of the 139 physicians surveyed able to identify the components.
In 2007, the ACSM updated the diagnostic guidelines, and the female athlete triad was defined as a spectrum of abnormalities in energy availability, menstrual function and bone mineral density, looking at the components as part of a spectrum ranging from normal to varying degrees of pathology. The female athlete no longer needs to demonstrate pathology and all three components of the triad in order to be diagnosed with the syndrome. (more…)
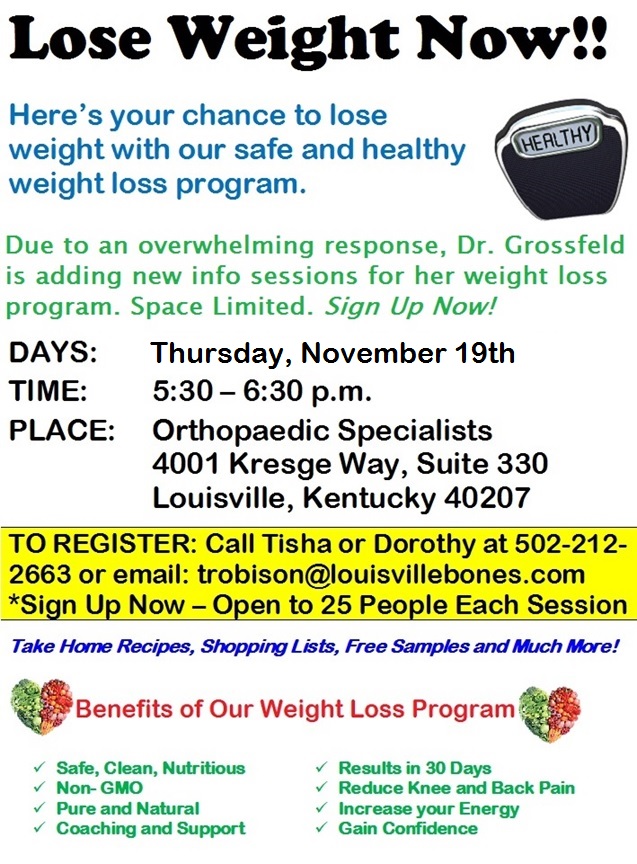
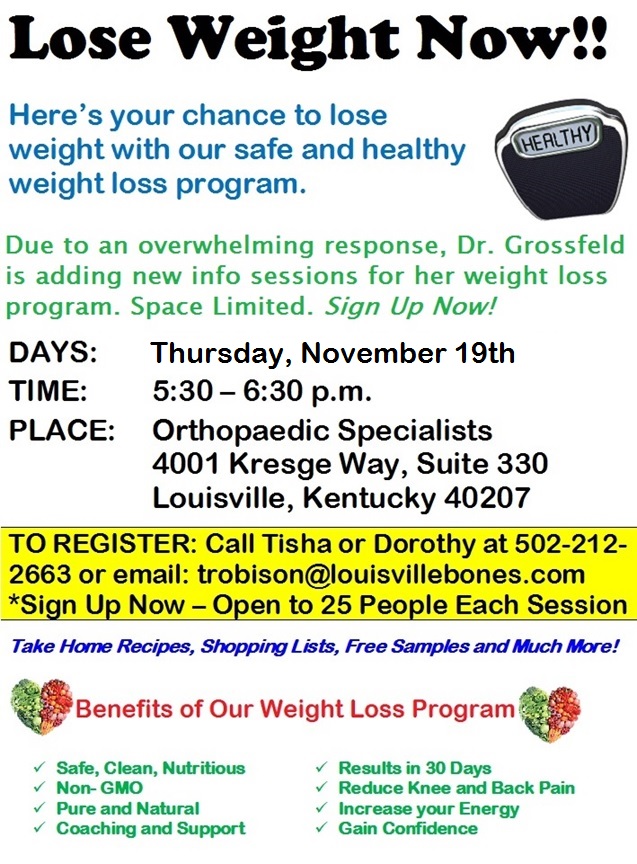
 Dr. Grossfeld recently attended a seminar on sports medicine given by Nick Sarantis, ATSC. The seminar was given to the fitness instructors at the Norton Commons YMCA. The purpose of the lecture was to talk about training methods.
Dr. Grossfeld recently attended a seminar on sports medicine given by Nick Sarantis, ATSC. The seminar was given to the fitness instructors at the Norton Commons YMCA. The purpose of the lecture was to talk about training methods.
Nick’s lecture was comprehensive and very informative. For example, one section of the lecture focused on giving excellent information on core strengthening. He stressed that the core muscles make up the foundation of the body and assist in injury prevention. He also emphasized that the core needs to be rehabbed after injury treatment. The foundation of our muscle function in sport starts at the core.
He also talked about certain core exercises that were bad to do such as crunches and Russians, because they put a significant amount of stress on the lumbar spine. He talked about other exercises that are excellent for the core and are safe such as planks.
The importance of strengthening your gluteus muscles was also emphasized because that also reinforces core strength.
Nick informed the fitness instructors at the Norton Commons YMCA about the benefits of working unilateral exercises. He also provided medical reasons why intervals are important to the workout regimen. And he offered guidance about how to organize exercises.
Exercise organization should be a progression, as explained by Nick. For example, it’s easier to do a box jump then jumping over a box. The progression in working out should start with the core, and then go to the upper body and finally, the lower body.
Dr. Grossfeld is a board member of the Norton Commons YMCA and a very active gym member. She (more…)
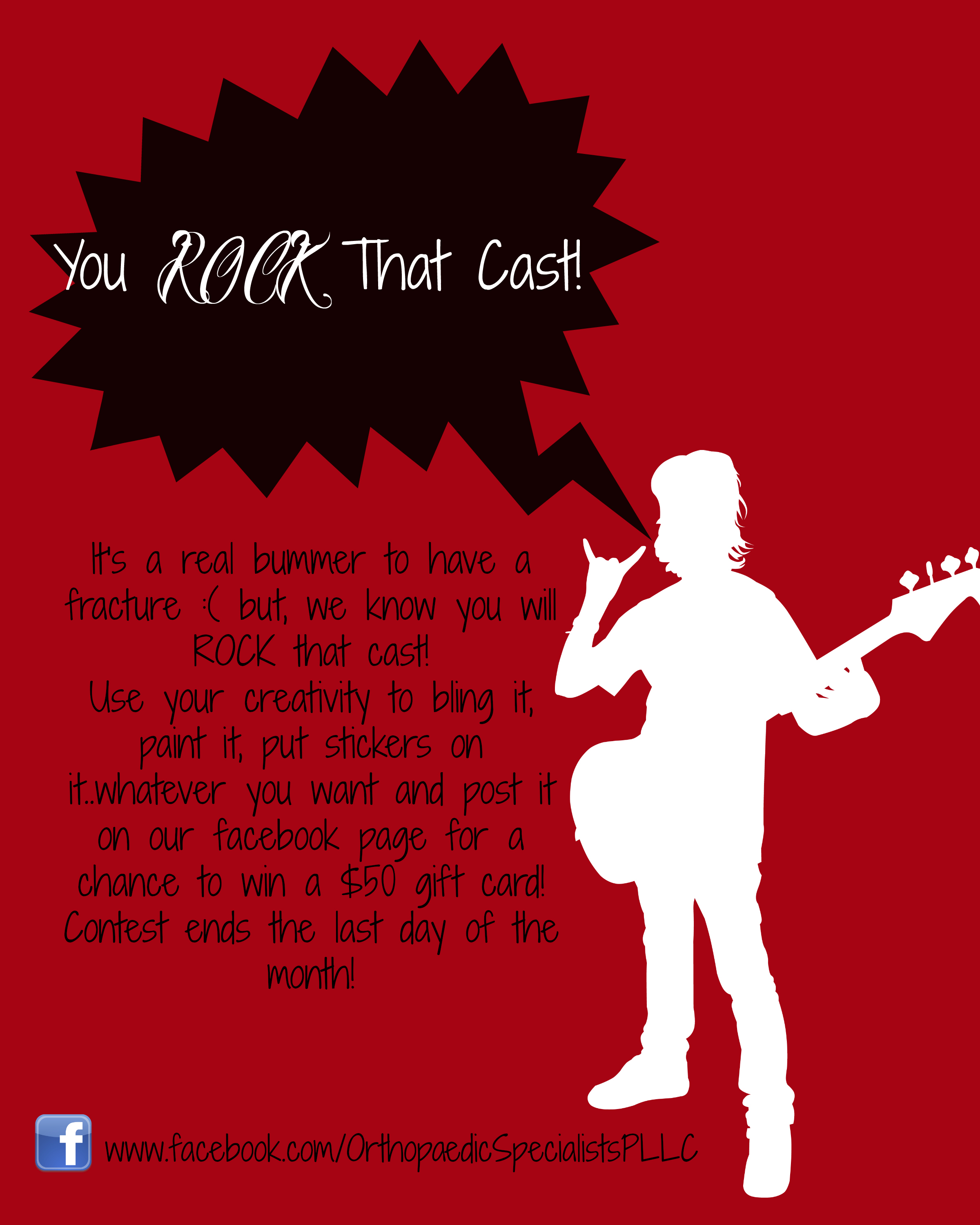
Are you a current patient at Orthopaedic Specialists? Are you currently wearing a cast? If you answered YES to both questions, we’ve got a great contest for you, complete with the opportunity to win a $50 gift card. Check out the flyer below for details and show us how you Rock that Cast!
 The entire team at Orthopaedic Specialists in Louisville, Kentucky, is dedicated to supporting Breast Cancer Awareness and to finding a CURE for breast cancer and every other type of cancer too. We’ve got some very personal reasons why we are wearing PINK this month that we’d like to share with you…
The entire team at Orthopaedic Specialists in Louisville, Kentucky, is dedicated to supporting Breast Cancer Awareness and to finding a CURE for breast cancer and every other type of cancer too. We’ve got some very personal reasons why we are wearing PINK this month that we’d like to share with you…
Lindsay Rhodus – “I wear pink! I wear pink for ALL the women who have fought and lost, I wear pink for ALL who have fought and won, I wear pink for ALL who will fight, I wear pink for families, friends, moms, dads, brothers, sisters, aunts, uncles, cousins, and co-workers, I wear pink TO FIND A CURE!”
Angel McDowell – “I wear pink to support the fight against breast cancer. I represent my mother who lost her fight with ovarian cancer 3 years ago, so I will give my all to support the fight to find a cure for cancer.”
Rhonda King – “I wear PINK in honor of my mom who passed away 12 years ago from Metastatic Breast Cancer at the age of 56.”
Dr. Stacie Grossfeld – “I wear pink for all my girlfriends that are fighting this disease. It is in support of them and their families, and to promote cancer research.”
Dorothy Cochran – “I wear Pink for my Grandma Dorothy who passed away 35 years ago after a very long battle. Although I have never had the opportunity to meet her, I know she was a fighter and I’m happy to have been named after her. I support the cure for her!”
Heather Hardiman – “I wear pink for my very good friend Ginny, she is a 2 time survivor!”
Angel Porter – “I wear pink for my “sis” Glenda!!”
Tisha Robison – “I wear pink for my aunts and friends who have gone through and will go through this battle. I wear pink to remind myself and others to do the testing and to never give up on the fight!”
Marti Spencer – “I wear pink for my very good friend Tammi Poole. She is the bravest woman I have ever met in my life. I watched her during her struggle and the effects it had on her mentally, physically, emotionally as well as the effect it had on her family. She was always positive, upbeat and STRONG!!! She is now in remission and has kicked Cancer’s tail!!! She is my Hero!!!!”
Jennifer Yocum – “I wear pink to support all women who are fighting this horrific disease and to remind all of us to perform monthly breast exams, get yearly exams by a physician and mammograms.”
Meghan Dawson – “I wear pink for Aunt Amy & Aunt Bridget who are both Breast Cancer survivors!”

World Spine Day is recognized annually on October 16 as a way to raise awareness about disorders of the spine and spine health. The spine is a very important part of your body. Learn more about your spine with the following facts.
the spine and spine health. The spine is a very important part of your body. Learn more about your spine with the following facts.
Arthritis affects millions of people around the world. And nearly 40 million Americans have some kind of arthritis including millions of children. Over 20 million people in the U.S. have osteoarthritis.
Osteoarthritis is a joint disease characterized by the degeneration of joint cartilage in your body. It can affect any of your joints including hands, hips and knees. Follow along to learn more important facts about osteoarthritis from Louisville orthopedic Dr. Stacie Grossfeld.
Your feet are responsible for many different functions. These flexible, complex structures are comprised of several different components including tendons, muscles, joints, bones and tissue. All of these important pieces work together to help us perform many different physical activities and navigate through life.
Foot health is extremely important for continuing an active and healthy lifestyle. It is easy to take your feet for granted until you experience some type of foot injury. Here are seven types of foot injuries that require special attention and treatment. While there are many different kinds of foot injuries, these tend to be some of the most common.

 Total hip replacement is an increasingly popular operation that can significantly improve the quality of the lives of the patients that undergo the procedure. A total hip replacement can significantly reduce pain, improve range of motion of the joint and lead to a more active life.
Total hip replacement is an increasingly popular operation that can significantly improve the quality of the lives of the patients that undergo the procedure. A total hip replacement can significantly reduce pain, improve range of motion of the joint and lead to a more active life.
On the other hand there are sometimes complications after total hip replacement that can lead to a poor result, and even require revision surgery. According to research by Drs. Mark Dwyer, Victor Goldberg and Glenn Wera, as reported in the July 2015 American Academy of Orthopaedic Surgeons (AAOS) journal, the most common complications of total hip replacement surgery that can lead to a poor result are: hip dislocation, infection and osteolysis (or the destruction/disappearance of bone tissue).
According to the researchers, there were approximately 332,000 total hip replacements in 2010 with a 3.9% dislocation rate. Risk factors for complications after total hip replacement can be divided into two major groups: 1) patient-related and 2) surgically-related.
Risk factors that are associated with complications following a total hip replacement include the following:
Surgery related risk factors associated with problems following a total hip replacement include the following:
Recent Comments