Descripción General de la Cirugía Labral / SLAP / Bankart
Especialistas Ortopédicos 502-212-2663
Stacie Grossfeld, M.D. / Bess Fley, PA-C

La reparación del labrum, reparación SLAP, y la cirugía de reconstrucción de Bankart se realizan como un procedimiento ambulatorio.
A su llegada al centro quirúrgico, primero se reunirá con la persona de registro para registrarlo. Luego lo llevarán de regreso al área preoperatoria y se reunirá con su equipo de enfermería.
Anestesia
La siguiente persona que conocerá es el médico de anestesia. En este momento, el anestesiólogo discutirá el proceso y abordará cualquier pregunta o inquietud que tenga sobre la anestesia. El anestesiólogo colocará un bloqueo nervioso para adormecer el hombro y el brazo. El medicamento anestésico durará 18 horas. Esta es una excelente manera de reducir el dolor postoperatorio. Incluso después de que el bloqueo nervioso desaparece, su nivel de dolor se reduce debido al efecto antidolor del bloqueo nervioso.
Después de colocar el bloqueo nervioso, usted irá a la sala de operaciones donde se realiza la reparación del labrum, la reparación SLAP y la cirugía de reconstrucción de Bankart. Luego, el anestesiólogo administrará una anestesia general, por lo que estará completamente dormido para el procedimiento. Usted puede ser intubado o no. Hay múltiples factores que determinan el tipo de anestesia. Su anestesiólogo discutirá eso con usted en detalle. Debido a que es una anestesia general, no escuchará ni verá nada de lo que sucede en la sala de operaciones.
Procedimiento quirúrgico
El Dr. Grossfeld realizará la reparación del labrum, SLAP, y Bankart artroscópicamente. Este procedimiento dura entre 45-60 minutos. Tenga en cuenta que después de regresar a la sala de operaciones, toma alrededor de 40-50 minutos irse a dormir y colocarse en la cama de la sala de operaciones, por lo que es posible que su familia no lo vea durante 2.5 horas, dependiendo de qué tan extenso sea el procedimiento quirúrgico y qué deba solucionarse.
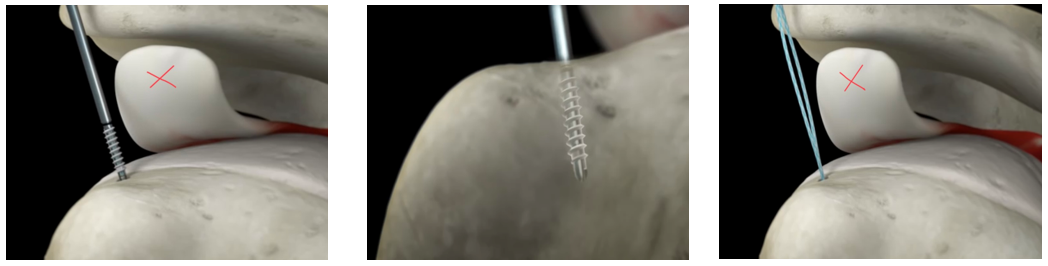
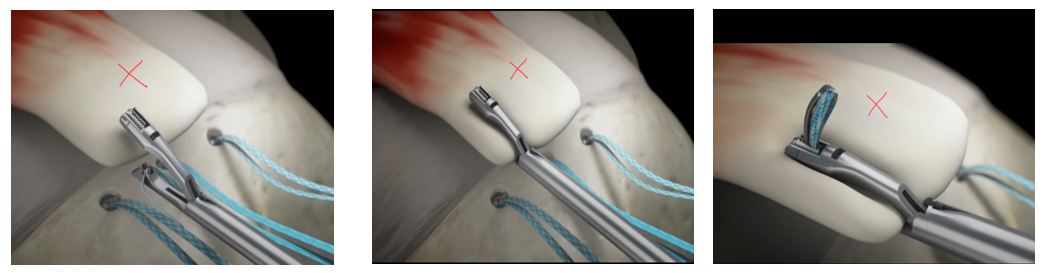
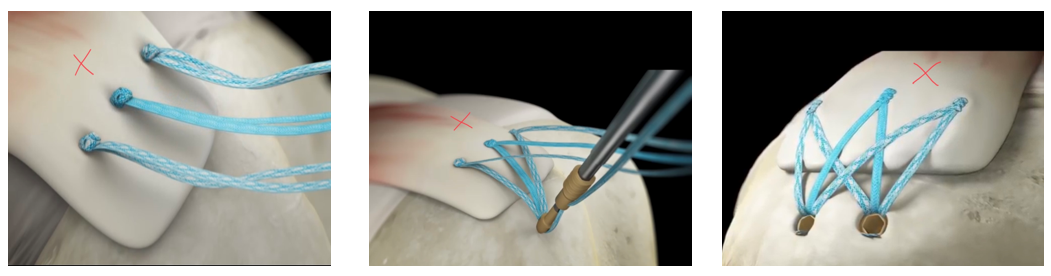
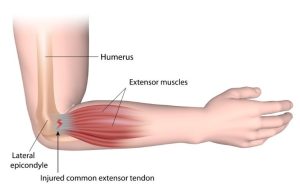
El Dr. Grossfeld hará de tres a cuatro incisiones pequeñas, que tienen menos de un centímetro de largo alrededor de la articulación del hombro. Ella colocará una pequeña cámara de alta definición, aproximadamente del tamaño de un lápiz, en la articulación del hombro. Después de insertar la cámara, se completa la inspección de toda la articulación del hombro. Se ve cada compartimento del hombro. Ella identificará dónde se encuentra el desgarro del labrum, SLAP, y Bankart. La reparación del labral/SLAP/Bankart se realiza colocando dos o más anclajes de sutura.
Los anclajes de sutura están hechos de un material óseo de tipo sintético, por lo que los anclajes se incorporarán realmente a su propio hueso. Unidos a la cabeza del anclaje de sutura están los puntos que se utilizan para reparar el labrum desgarrado. Los anclajes de sutura se colocan en el hueso que luego “ancla la sutura” y las suturas se cosen alrededor del labrum desgarrado. Los nudos se atan tirando del labrum desgarrado hacia el hueso donde estaba unido antes de que ocurriera el desgarro.
Si hay espolones óseos, se eliminarán con una pequeña herramienta que es similar a una herramienta Dremel. Si se extirpan los espolones óseos, el procedimiento se denomina descompresión subacromial y/o escisión de la articulación AC.
Al final de la cirugía, el sitio de la incisión/sitios portales se cierran con una sutura de color azul llamada Prolene. Las suturas se retirarán cuando lo vean en el consultorio entre 10 y 14 días después de la cirugía. No deje que las suturas o el sitio de la incisión se mojen. Puede limpiar los sitios de incisión con peróxido. Usted recibió instrucciones postoperatorias detalladas el día de la cirugía que explicarán el cuidado postoperatorio de la herida.
Al salir de la sala de operaciones, se le colocará una gasa de 4 x 4 sobre los sitios de incisión, seguida de almohadillas ABD, que son un apósito esponjoso más grande, seguido de cinta quirúrgica. Su cabestrillo de hombro especializado se colocará en la sala de operaciones.
Recibirá un conjunto detallado de instrucciones sobre el cuidado de la herida al ser dado de alta del centro quirúrgico.
Noche de Cirugía
Es muy importante que te mantengas al tanto del dolor. El hielo es clave. Es muy importante usar hielo tanto como sea posible. El Dr. Grossfeld recomienda el uso continuo de hielo durante todo el día. La regla es que no puedes usar demasiado hielo. Ya sea una unidad Polar Care, una bolsa de hielo o una bolsa de guisantes o maíz congelados: úselo continuamente durante 6-7 días después de la cirugía.
Tenemos una unidad Polar Care que se puede comprar a través de nuestra oficina. Básicamente es una máquina de hielo motorizada que tiene una envoltura de neopreno que se coloca sobre el hombro operatorio. Es un refrigerador que está lleno de hielo y agua. Sugerimos congelar 8 botellas de agua llenas de agua. Coloque cuatro de las botellas congeladas en la máquina y luego vierta agua alrededor de las botellas congeladas. Cuando las botellas se descongelen, cámbielas por las otras cuatro botellas de agua congelada que están en su congelador.
La unidad Polar Care tiene una manguera que se conecta a una envoltura de neopreno que rodea el hombro y empujará el agua helada a través de la envoltura de neopreno durante un máximo de nueve horas. De hecho, le recomendamos que use hielo durante todo el día. Es la mejor fuente de control del dolor y ayuda a reducir la hinchazón.
Ella recomienda que configure su despertador y tome su medicamento para el dolor cada 4 a 6 horas durante las primeras 24 horas para mantenerse al tanto de su dolor. Agregar 800 mg de Motrin cada 6 horas o Meloxicam 15 mg cada 24 horas puede ayudar a controlar el dolor. No use Motrin o Meloxicam si está tomando anticoagulantes o tiene antecedentes de úlceras estomacales o enfermedad renal.
Puede ser más cómodo dormir en posición semi vertical. Dormir en un sillón reclinable o usar muchas almohadas para apoyar el hombro será más cómodo. Algunas personas dormirán en un sillón reclinable hasta 4 semanas después de la reparación del labrum / reparación SLAP / y la cirugía de reconstrucción Bankart. Cuando está acostado en la cama, permite que su hombro ruede hacia atrás y tira de la reparación, lo que puede causar dolor.
Uso de cabestrillo
Usted se despertará en la sala de recuperación con el cabestrillo en su lugar. Puede quitarse el cabestrillo siempre y cuando coloque el brazo contra el abdomen. El Dr. Grossfeld recomienda que duerma en el cabestrillo porque evitará que su brazo se mueva durante la noche.
Apósito quirúrgico
Al final de la cirugía, el Dr. Grossfeld, se pondrá un vendaje. El apósito es un montón de almohadillas de gasa 4×4, una almohadilla abd y luego una cinta quirúrgica especial va encima del apósito.
Consulte sus órdenes postoperatorias que recibirá el día de la cirugía para conocer los detalles del cambio de vendaje.
Los apósitos para comprar antes del día de su cirugía son: de diez a 15: almohadillas de gasa 4×4, cinta médica de papel, tiritas a prueba de agua y peróxido.
Primera visita postoperatoria
Su primera visita postoperatoria será de 10 a 14 días después de la cirugía. Usted será visto en la oficina en ese momento y le quitarán las suturas. El Dr. Grossfeld o Bess Fley, PA-C revisarán sus fotos quirúrgicas y responderán cualquier pregunta. En esta visita lo más probable es que se ordene fisioterapia. Por lo general, la fisioterapia es solo una o dos veces por semana durante las primeras seis semanas. El TP variará de persona a persona según el tamaño del desgarro y la calidad de la reparación.
Fisioterapia
Se le darán ejercicios para hacer post operatorio. Hay un enlace en sus instrucciones / órdenes postoperatorias que recibirá el día de su reparación del labrum, reparación SLAP y cirugía de reconstrucción Bankart. El enlace le mostrará cómo hacer algunos ejercicios postoperatorios suaves. En la primera visita postoperatoria, también deberá comprar un juego de poleas (puede comprar en nuestra oficina por $ 20) para permitirle trabajar en ejercicios de rango de movimiento pasivo en casa.
PT se divide en dos o tres bloques de 6 semanas, dependiendo de qué tan extensa sea la reparación.
Las primeras 6 semanas asistirás una o dos veces por semana para trabajar en ejercicios suaves de ROM pasiva.
Las segundas seis semanas, la terapia implica un rango activo de movimiento del hombro con un fortalecimiento suave. Asistirá de 1 a 3 veces a la semana, dependiendo de su reparación y otros factores.
Las terceras seis semanas de fisioterapia implican aumentar el rango de movimiento y fortalecer aún más.
Esto es aproximadamente una recuperación de cuatro a cinco meses antes de que vuelva a sus actividades normales que involucran el hombro operado.
Conducción
La mayoría de las personas comenzarán a conducir una vez que hayan dejado de tomar todos los analgésicos. Una vez que se inicia la conducción, su cabestrillo debe quitarse mientras conduce. Se recomienda que coloque su mano en el lado quirúrgico en la parte inferior del volante y su mano no quirúrgica en la parte superior del volante para hacer la mayor parte del trabajo.
Regreso al trabajo
Si trabaja en un trabajo de tipo laboral, lo más probable es que no regrese a ese trabajo hasta que sea liberado al 100%. Si su empleador tiene opciones de trabajo ligero, lo más probable es que sea liberado entre dos y cuatro semanas de regreso al trabajo ligero. Por lo general, el trabajo ligero no requiere el uso del lado quirúrgico / el lado en el que se realiza la reparación de labros, la reparación de BOFETADAS y la cirugía de reconstrucción de Bankart, excepto para tareas simples como usar una computadora o contestar un teléfono. Tenga en cuenta que si todavía está tomando analgésicos, no puede conducir un vehículo.
Si tiene un trabajo de oficina, lo más probable es que pueda volver a trabajar entre dos y cuatro semanas. El regreso al trabajo también dependía del nivel de dolor. Algunas personas tienen mucho dolor después de la reparación del labrum, la reparación de SLAP y la cirugía de reconstrucción de Bankart, algunas personas tienen muy poco. El dolor es muy personal, y le proporcionaremos medicamentos para el dolor para cubrir su dolor según sea necesario. Se administrarán analgésicos durante un período de tiempo apropiado.
FMLA y papeleo de discapacidad
Nuestra oficina ofrece el servicio de completar el papeleo para FMLA y / o discapacidad por una tarifa de $ 40, por conjunto de documentos, y se completa en el orden en que se recibe, generalmente toma de 7 a 10 días hábiles. Todas las solicitudes deben originarse con su empleador, ya que su elegibilidad para FMLA y / o discapacidad se basa en sus beneficios con su empleador. Si bien cada paciente es único, hacemos todo lo posible para estimar el tiempo de recuperación y, a menudo, sobreestimamos la cantidad de tiempo para evitar un lapso en los beneficios y / o requerir papeleo adicional. Muchas veces las compañías de discapacidad requieren actualizaciones después de cada cita. Es responsabilidad del paciente comunicar esta solicitud a la oficina. Las actualizaciones no se completan automáticamente. Cualquier pregunta al respecto puede dirigirse a Dorothy.

 Ever since they outgrew their Hikes Point location, this Fern Creek lot has given more space to expand the collection of flowers and plants that Chris and Bill have accrued over the years. From the first daylily that Bill Schardein won with at a club meeting in 1989 to over 850 named cultivars in 20 garden settings throughout their property, the couple, even at the ages of 76 and 72, have flourished in their gardening endeavors. This came to a head in 1999, when they were approved by the regional officers to be added to the National Registry for Daylilies, where they have been registered since.
Ever since they outgrew their Hikes Point location, this Fern Creek lot has given more space to expand the collection of flowers and plants that Chris and Bill have accrued over the years. From the first daylily that Bill Schardein won with at a club meeting in 1989 to over 850 named cultivars in 20 garden settings throughout their property, the couple, even at the ages of 76 and 72, have flourished in their gardening endeavors. This came to a head in 1999, when they were approved by the regional officers to be added to the National Registry for Daylilies, where they have been registered since.
 While it disrupted her sleep and kept her from doing what she needed to in the garden, as long as she did not lift too much weight, Chris was able to get a few of her tasks done without her hand pain to worry about.
While it disrupted her sleep and kept her from doing what she needed to in the garden, as long as she did not lift too much weight, Chris was able to get a few of her tasks done without her hand pain to worry about.







Recent Comments