Meet this month’s patient in the spotlight, Joyce Koch!

If you were previously a student at St. Agnes, Assumption High School, or Presentation Academy, then Joyce’s name might be familiar. Having been a teacher since 1968, with 29 years spent at Assumption High School and the other 24 spent between Presentation Academy and St. Agnes teaching English and math, Joyce has had a long career in the Louisville educational field.
What makes Joyce a true spotlight patient, though, is that she sought opportunities to become better and initiated changes in her community that benefited the students she taught, the teachers she worked alongside, and her school as a whole.
When mainstream technology and computers became popular in the early 80’s, Joyce saw it as an opportunity to grow and took it, obtaining a degree in computer education at Spalding University along with her higher education degrees she already had in other areas. This led her to become first the technology coordinator at Assumption, and then the IT Director 9 years later, where she led the school in becoming leaders in educational technology for 20 years.

Now retired since 2021, Joyce would have liked to have spent her last few years working as she always had: with pep, passion and without any pain. For much of her life, Joyce was able to enjoy being a mother, teaching, reading, yoga, stretching, and walking for miles without any difficulties. In fact, she belongs to 2 different book clubs, listens to audiobooks regularly, and lives her life with the motto that, “You always have time for the things you put first,” – something that she always managed to apply to her stretching routine! She loves walking through Louisville’s myriad of beautiful parks, and was even in the habit of walking the mile from her home to school every day when she was working at Assumption High School.
Her time doing what she loved was cut short unexpectedly, though, when she experienced a series of injuries that put her out of commission in 2019.
Joyce’s Story
One After Another
Before her recent injuries, Joyce’s relationship with Dr. Grossfeld and Orthopaedic Specialists dates back to 2005, when an instructional yoga video with her daughters triggered an arthritis flair-up in her right knee. This particular injury didn’t seem all that serious – when Dr. Grossfeld headed her PT, her pain went away and she had no complications until 2019, when her other knee began giving out on her. Deciding to take her issue to Dr. Grossfeld again, she made an appointment, but before she was able to address her knee, she was rear-ended in a car accident and began experiencing back pain that was much worse than her knee pain.
Dr. Grossfeld was able to address her pain and injuries with medications and another bout of physical therapy, this time for her back, but before she experienced relief, less than a month from her accident, Joyce was rear-ended again, which worsened her condition to the point that standing and walking caused her severe pain. Now using a cane and having difficulties sleeping that also led to a pop-up case of temporomandibular disorder (TMD), Joyce felt it was time to take a leave of absence so that she could focus on resolving her pain. Dr. Grossfeld was able to send her to a pain specialist, who diagnosed a pinched nerve in her vertebrae that would require a series of treatments over the course of a few weeks.
But, in the midst of her pain, the world was hit by the pandemic and Joyce’s pain center closed, leaving her without treatment until June of 2020. Even struggling with pain, Joyce managed to contribute to Assumption’s success during the age of online learning before her injury ever happened – she’d had the foresight to begin teaching the teachers about online instruction and how to navigate that world a whole year before, and her colleagues and students had never been more grateful, even as she was on leave.
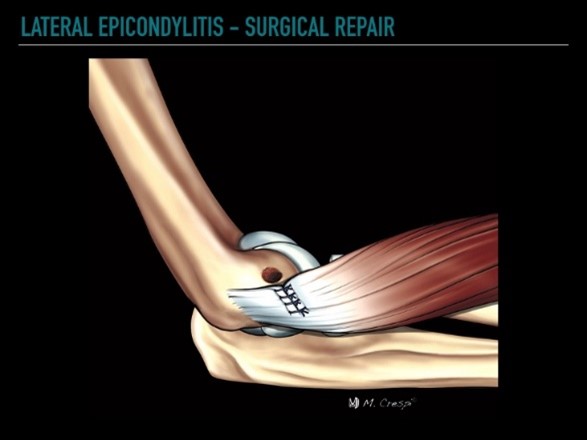
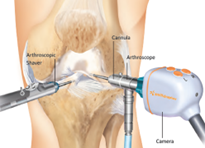
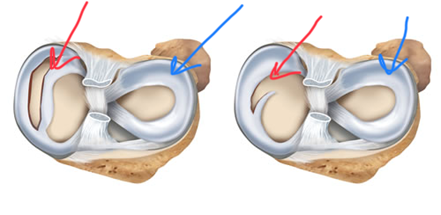
By the time she was able to receive treatment, Joyce’s back pain had caused her knees to worsen without the ability to walk or keep stretching, which led to her right knee replacement in 2021. But, as her right knee improved, Joyce found that her left knee’s development was moving in the opposite direction. Sure enough, Dr. Grossfeld completed a knee arthroscopy surgery to remove a meniscal tear in her left knee, which fixed her pain until her arthritis came back and she was sent to get her left knee replaced.
Recovery and Joyce Today
From her original concerns until her last knee replacement surgery, Joyce says that her recovery took around a total of 3 years. At the height of her pain, Joyce felt unable to do most things that she loved, including walking, stretching, and even cooking! While she tried to supplement some parts, like taking up water-walking at Dr. Grossfeld’s advice, the lack of sleep and weakness her injuries caused left her mood suffering.
These factors combined with the effects of the pandemic caused her retirement to come earlier than she intended, but it allowed her to put 100% into getting better and back to a quality of life that was as close to where she was before as possible.

(Pictured Above: Mary Lang, President of Assumption High School, and Joyce Koch on March 22, 2023, when she was awarded a “Distinguished Educator” trophy and an honorary diploma.)
“Dr. Grossfeld truly listens to what you are feeling and hones in on the correct plan of action. She and her staff are caring, compassionate people treating the whole person, not simply one offending joint. I have recommended them to my family and friends who feel the same way about them as I,” Joyce says, having done plenty of physical therapy and treatments with Dr. Grossfeld throughout the time she was injured and recovering.
With the help of Dr. Grossfeld’s diagnoses and recovery methods, now, with the back pain under control and both knees replaced, Joyce is back to stretching first thing in the morning for 20-30 minutes to start her day and is able to walk 3 or 4 miles a day as she had before. Sleeping through the night and the ability to cook homemade meals every night once more has become normal, and Joyce says that the work was difficult in many ways, but that she’s grateful to be back to doing what she loves!
If you or someone you love has suffered a knee or back injury in the Louisville, Kentucky-area, board certified sports medicine physician Dr. Stacie Grossfeld at Orthopaedic Specialists PLLC can help. Orthopaedic Specialists PLLC is accepting new patients, and same day appointments are available. For additional information or to schedule an appointment, please contact Orthopaedic Specialists PLLC today at 502-212-2663.






Recent Comments