Descripción General de la Cirugía del Manguito Rotador
Especialistas Ortopédicos 502-212-2663
Stacie Grossfeld, M.D. / Bess Fley, PA-C
La cirugía del manguito rotador se realiza como un procedimiento ambulatorio.
- No coma ni beba después del tiempo dado por el personal del Dr. Grossfeld
- Use ropa holgada
- Traiga información del seguro e identificación con foto
- Lista de medicamentos y alergias a medicamentos
- Haga arreglos para que alguien conduzca a casa después del procedimiento
A su llegada al centro de cirugía, primero se reunirá con la persona de registro para registrarlo. Luego lo llevarán de regreso al área preoperatoria y se reunirá con su equipo de enfermería. Se medirán los signos vitales, como la presión arterial y la temperatura.
Se proporcionará una bata de hospital limpia. Todas las joyas, dentaduras postizas, lentes de contacto y esmalte de uñas deben ser quitados. Se iniciará una vía intravenosa para administrarle líquidos y medicamentos durante y después del procedimiento. Su hombro será frotado y afeitado en preparación para la cirugía. Un anestesiólogo discutirá el tipo de anestesia que se utilizará. El Dr. Grossfeld confirmará e inicializará el sitio quirúrgico correcto con un rotulador.
Anestesia
Antes del procedimiento, se reunirá con el anestesiólogo. En ese momento, discutirán su historial médico / de anestesia pasada con usted. El anestesiólogo colocará un bloqueo nervioso para adormecer el hombro y el brazo. El medicamento anestésico durará 18 horas. Esta es una excelente manera de reducir el dolor postoperatorio. Incluso después de que el bloqueo nervioso desaparece, su nivel de dolor se reduce debido al efecto antidolor del bloqueo nervioso.
Después de colocar el bloqueo nervioso, usted irá al quirófano donde se realiza la cirugía. El anestesiólogo administrará una anestesia general, por lo que usted está completamente dormido para el procedimiento. Usted no oirá ni verá nada que suceda en la sala de operaciones.
Procedimiento quirúrgico
El Dr. Grossfeld realizará la reparación del manguito rotador artroscópicamente. Este procedimiento dura entre 45-90 minutos. Después de regresar a la sala de operaciones, toma alrededor de 40-50 minutos para irse a dormir y colocarse en la cama de la sala de operaciones, por lo que es posible que su familia no lo vea durante 2.5 horas, dependiendo de qué tan extenso sea el procedimiento quirúrgico. El Dr. Grossfeld hará de cinco a seis incisiones pequeñas que miden menos de 1/2 pulgada de largo alrededor de la articulación del hombro. Se colocará una pequeña cámara de alta definición, aproximadamente del tamaño de un lápiz, en la articulación del hombro. Después de insertar la cámara, se completa la inspección de toda la articulación del hombro. Se ve cada compartimento del hombro. Se identificará la ubicación del desgarro del manguito rotador. Si hay espolones óseos, se eliminarán. La extirpación del espolón óseo se denomina descompresión subacromial y/o escisión de la articulación AC. Cualquier otro hallazgo anormal también se abordará en el momento de la cirugía y la reparación.

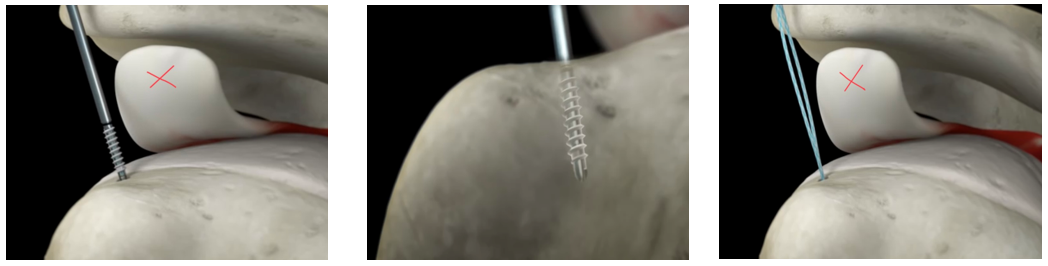
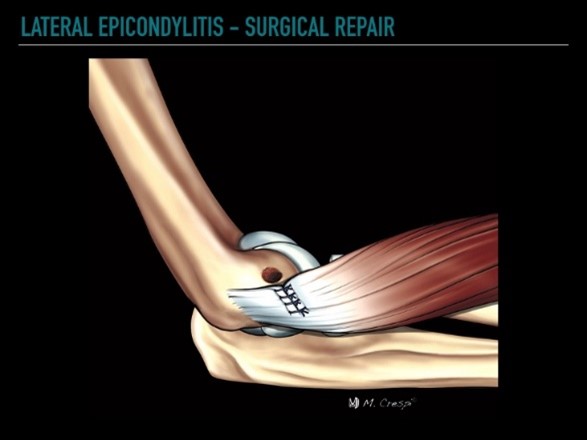
La reparación del manguito rotador se realiza colocando tres o cuatro anclajes de sutura en el hueso del hombro.
Los anclajes de sutura están hechos de un hueso sintético, los anclajes se incorporarán a su propio hueso. La imagen de la izquierda es un anclaje de sutura utilizado para reparar los manguitos rotadores rotos.
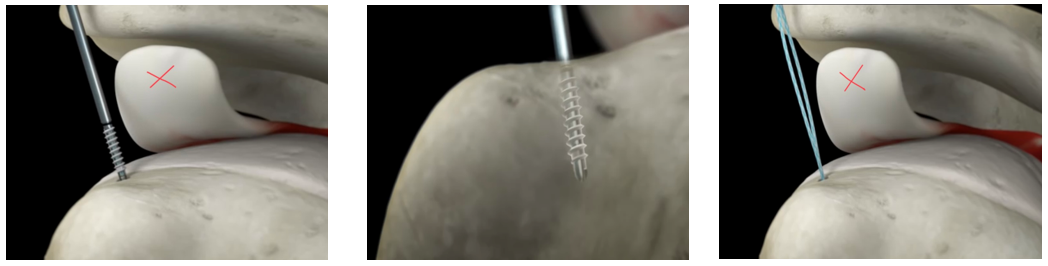
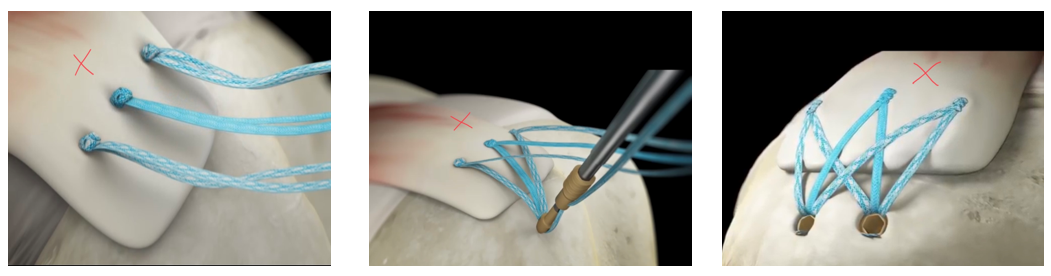
La primera imagen de arriba revela el anclaje atornillado en el hueso del hombro (la x marca el tendón del manguito rotador desgarrado). La imagen del medio muestra el anclaje de sutura asegurado en el hueso del hombro. La última imagen muestra cómo las suturas ahora están “ancladas” en el húmero y listas para ser suturadas a través del tendón del manguito rotador desgarrado.
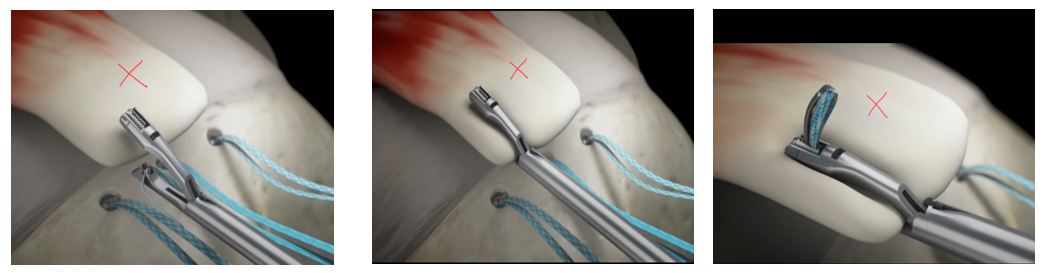
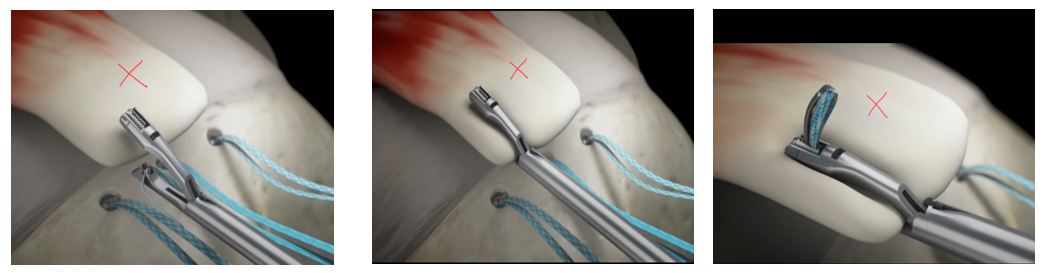
Las imágenes de arriba muestran cómo se cose la sutura a través del tendón del manguito rotador desgarrado. Las suturas se pegan a través del tendón del manguito rotador desgarrado con un instrumento especial diseñado específicamente para la tarea.
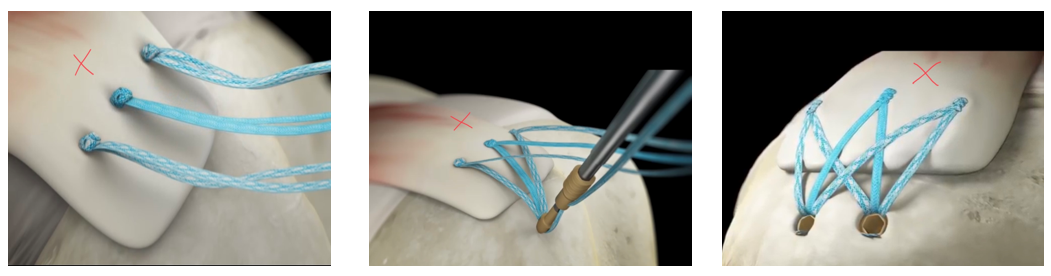
Las tres imágenes de arriba muestran los nudos que están atados para sostener el tendón desgarrado contra el hueso del hombro. La segunda y tercera imagen muestran el segundo juego de anclajes que refuerzan la reparación. La imagen final es un tendón del manguito rotador reparado.
El tendón reparado se volverá a unir al hueso. Las suturas están ahí para sostener el tendón de forma segura contra el hueso mientras se lleva a cabo el proceso de curación.
Si hay espolones óseos, se eliminarán con una pequeña herramienta similar a un Dremel.
El sitio de incisión/sitios portal se cierran con una sutura de color azul llamada Prolene. Las suturas se retirarán cuando lo vean en el consultorio entre 10 y 14 días después de la cirugía.
Al salir de la sala de operaciones, se le colocará una gasa de 4 x 4 sobre los sitios de incisión, seguida de almohadillas ABD que son un apósito esponjoso más grande, seguido de cinta quirúrgica. Su cabstrillo de hombro especializado se instalará en la sala de operaciones.
Recibirá un conjunto detallado de instrucciones sobre el cuidado de la herida al ser dado de alta del centro quirúrgico.
Noche de Cirugía
Es muy importante que te mantengas al tanto del dolor. El hielo es clave. Use hielo tanto como sea posible. El Dr. Grossfeld recomienda el uso continuo de hielo durante todo el día. La regla es que no puedes usar demasiado hielo. Ya sea una unidad Polar Care o bolsas de guisantes congelados: úselo continuamente durante 6-7 días después de la cirugía.
Las unidades Polar Care están disponibles para la compra de especialistas ortopédicos por $150.00. No están cubiertos por el seguro. Polar Care es una máquina de hielo motorizada que consiste en una envoltura de neopreno que se coloca sobre el hombro operatorio y un refrigerador que se llena con hielo y agua. Una manguera se conecta a una envoltura de neopreno que rodea el hombro y empujará el agua a través de la envoltura de neopreno durante un máximo de nueve horas. Por favor, congele ocho botellas de agua antes de su cirugía. Coloca cuatro botellas de agua congelada en la unidad Polar Care. Luego, llénate con agua. Esto mantendrá el agua más fría por más tiempo. Cuando las cuatro botellas de agua se descongelen, reemplácelas con cuatro botellas congeladas más y vuelva a colocar las botellas descongeladas en el congelador. Continúe repitiendo este ciclo. Use hielo durante todo el día, incluso cuando duerma. El hielo es la mejor fuente de control del dolor y la hinchazón.
Configure su despertador y tome su medicamento para el dolor cada 4 a 6 horas durante las primeras 24 horas para mantenerse al tanto de su dolor. Agregar 800 mg de Motrin cada 6 horas O Meloxicam 15 mg cada 24 horas también puede ayudar a reducir el dolor postoperatorio. No use Motrin o Meloxicam si está tomando anticoagulantes o tiene antecedentes de úlceras estomacales o enfermedad renal
Dormir en un sillón reclinable, en posición vertical o usar muchas almohadas para apoyar el hombro será más cómodo. Algunas personas dormirán en un sillón reclinable hasta 4 semanas después de la cirugía. Acostarse en la cama permite que su hombro ruede hacia atrás, lo que tira de la reparación y causará dolor.
Uso de cabestrillo
Se despertará en la sala de recuperación con el cabestrillo puesto. Ocasionalmente, puede quitarse el cabestrillo mientras descansa (NO dormido), siempre y cuando coloque el brazo contra el vientre. Cuando duerme, el cabestrillo debe estar puesto.
Apósito quirúrgico
Se colocará un vendaje, que consiste en almohadillas de gasa 4×4, almohadillas ABD y cinta quirúrgica especial en el sitio quirúrgico (s). Consulte las órdenes postoperatorias que se le dieron el día de la cirugía para conocer los detalles del cambio de vendaje.
Los apósitos para comprar antes del día de la cirugía son: 10-15 almohadillas de gasa 4×4, una envoltura as extra de 6 pulgadas, peróxido, cinta de papel y curitas impermeables. Los kits están disponibles para su compra en Orthopaedic Specialists.
Primera visita postoperatoria
Su primera visita postoperatoria será de 10 a 14 días después de la cirugía. Las suturas serán retiradas por un asistente. El Dr. Grossfeld o Bess Fley, PA-C revisarán su informe operativo, fotos quirúrgicas y responderán cualquier pregunta restante. Se puede ordenar fisioterapia. Por lo general, la fisioterapia es solo una o dos veces por semana durante las primeras seis semanas. El TP variará de persona a persona según el tamaño del desgarro y la calidad de la reparación.
Ejercicios en el hogar y fisioterapia
Se darán ejercicios para hacer post operatorio. Un enlace a estos ejercicios está en las instrucciones / órdenes postoperatorias dadas el día de su cirugía. El enlace le mostrará cómo hacer algunos ejercicios postoperatorios suaves. Un juego de poleas, que se puede comprar en nuestra oficina por $ 20, le permite trabajar en ejercicios de rango de movimiento pasivo en casa después de la cirugía.
La fisioterapia se divide en tres bloques de 6 semanas. Las primeras 6 semanas asistirás una vez a la semana para trabajar en ejercicios suaves de rango de movimiento pasivo.
La segunda terapia de seis semanas implica un rango activo de movimiento del hombro con un fortalecimiento suave. Asistirá de 1 a 3 veces a la semana, dependiendo de su reparación y otros factores.
Las terceras seis semanas de fisioterapia implican aumentar el rango de movimiento y fortalecer aún más. Esto es aproximadamente una recuperación de cinco a seis meses antes de que vuelva a sus actividades normales que involucran el hombro operado.
Conducción
Puede comenzar a conducir después de dejar de tomar todos los analgésicos narcóticos. Una vez que comience a conducir, su cabestrillo debe quitarse mientras conduce. Se recomienda colocar su mano, del lado operatorio, en la parte inferior del volante y su mano no quirúrgica en la parte superior del volante para hacer la mayor parte del trabajo.
Regreso al trabajo
Si trabaja en un trabajo de tipo laboral, es posible que no regrese hasta que sea liberado al 100%. Sin embargo, si su empleador puede acomodar opciones de trabajo ligero, puede regresar tan pronto como dos a cuatro semanas después de la cirugía. Las opciones de trabajo ligero no requieren el uso de la extremidad quirúrgica, excepto para tareas simples como el uso de una computadora.
Si tiene un trabajo de oficina, lo más probable es que pueda volver a trabajar entre dos y cuatro semanas. El regreso al trabajo también depende del nivel de dolor. Algunas personas tienen mucho dolor después de esta cirugía en particular, algunas personas tienen muy poco. El dolor es muy personal, y le proporcionaremos analgésicos de acuerdo con nuestra política de oficina y la ley del estado de Kentucky. Los medicamentos para el dolor se recetarán adecuadamente en cuanto a dosis, cantidad y tiempo.
FMLA y papeleo de discapacidad
Nuestra oficina ofrece el servicio de completar el papeleo para FMLA y / o discapacidad por una tarifa de $ 40, por conjunto de documentos, y se completa en el orden en que se recibe, generalmente toma de 7 a 10 días hábiles. Todas las solicitudes deben originarse con su empleador, ya que su elegibilidad para FMLA y / o discapacidad se basa en sus beneficios con su empleador. Si bien cada paciente es único, hacemos todo lo posible para estimar el tiempo de recuperación y, a menudo, sobreestimamos la cantidad de tiempo para evitar un lapso en los beneficios y / o requerir papeleo adicional. Muchas veces las compañías de discapacidad requieren actualizaciones después de cada cita. Es responsabilidad del paciente comunicar esta solicitud a la oficina. Las actualizaciones no se completan automáticamente. Cualquier pregunta al respecto puede dirigirse a Dorothy.





 Ever since they outgrew their Hikes Point location, this Fern Creek lot has given more space to expand the collection of flowers and plants that Chris and Bill have accrued over the years. From the first daylily that Bill Schardein won with at a club meeting in 1989 to over 850 named cultivars in 20 garden settings throughout their property, the couple, even at the ages of 76 and 72, have flourished in their gardening endeavors. This came to a head in 1999, when they were approved by the regional officers to be added to the
Ever since they outgrew their Hikes Point location, this Fern Creek lot has given more space to expand the collection of flowers and plants that Chris and Bill have accrued over the years. From the first daylily that Bill Schardein won with at a club meeting in 1989 to over 850 named cultivars in 20 garden settings throughout their property, the couple, even at the ages of 76 and 72, have flourished in their gardening endeavors. This came to a head in 1999, when they were approved by the regional officers to be added to the 
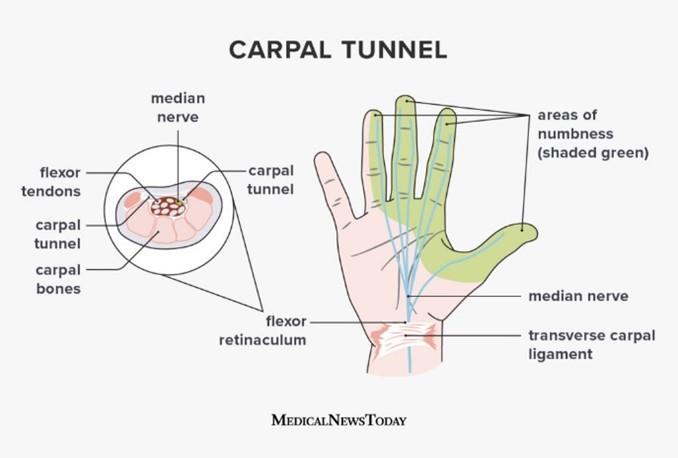
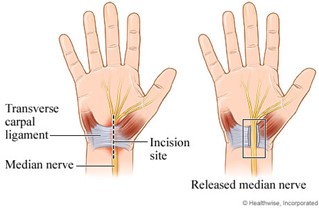
 While it disrupted her sleep and kept her from doing what she needed to in the garden, as long as she did not lift too much weight, Chris was able to get a few of her tasks done without her hand pain to worry about.
While it disrupted her sleep and kept her from doing what she needed to in the garden, as long as she did not lift too much weight, Chris was able to get a few of her tasks done without her hand pain to worry about.



Recent Comments