The rotator cuff is a group of four tendons that are located in the shoulder. When a portion of the tendon tears, it can produce pain and disability. This injury is quite common and often requires surgical repair. Here are some of the questions I get asked daily as an orthopaedic surgeon:
Rotator Cuff Tear Symptoms
Above all, the most common symptom of a torn rotator cuff is night pain. Secondly, pain with overhead activity or there is difficulty with bringing you arm behind your back, such as putting your wallet in your back pocket or zipping up a dress.
Where is the Pain From a Torn Rotator Cuff Tear Located?
The pain from a rotator cuff tear is located on the lateral aspect of the arm. Pain is in the area of the deltoid muscle. In addition, the pain radiates down the arm, sometimes to the elbow.
What Causes the Rotator Cuff to Tear?
Most rotator cuff tears occur with age. Therefore, rotator cuff tears tend to be degenerative in nature. Traumatic cuff tears are less common. Traumatic cuff tears are closely associated with shoulder dislocations in people over age 60. In addition, a fall that results in a person landing on a flexed elbow can also traumatically tear the rotator cuff. However, it is rare to tear your rotator cuff if you are under age 40. Most cuff tears occurs in patients 50 years or older, because as we age our rotator cuffs weaken. They can tear with just normal activities of daily living!
Key Findings on Physical Examination of a Rotator Cuff Tear
Key findings on physical examination of a rotator cuff tear is pain located over the lateral side of the upper arm. The doctor will perform physical tests that include a Neer Test and Kennedy-Hawkins Test, as well as placing the shoulder through a range of motion. In addition, strength will be tested, pulses evaluated and sensation tested.

The image reveals the key physical tests to perform to document a rotator cuff tear.
Imaging needed to Diagnosis a Rotator Cuff Tear
The initial imaging is a standard shoulder x-ray. If the x-ray does not reveal the source of shoulder pain a MRI will be obtained . A MRI will show soft tissue, bone edema, and detailed areas of arthritis that plain x-rays cannot reveal. However, if the patient has a pacemaker, MRI can not be obtained. In addition, it is difficult for claustrophobic patients to undergo a that study.
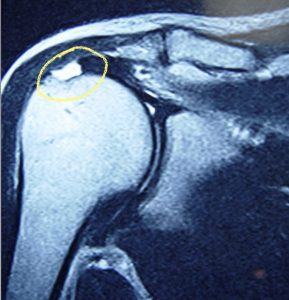
The circle reveals where the rotator cuff tear is located on the MRI.
Treatment of Rotator Cuff Tears
The primary treatment option for a repairable rotator cuff tear is surgery. There are some rotator cuff tears that are not reparable; Massive tears with fatty atrophy and old chronic tears with significant retraction are not amendable to surgery.
Surgery is outpatient and arthroscopic. The surgery is relatively low risk. Smokers put the repair at risk for not healing, as the nicotine in cigarettes inhibits healing. A massive tear greater than four centimeters has a high rate of non-healing. In addition, tears were the rotator cuff is thin, avascular and friable have a difficult time healing even after the perfect surgical reconstruction.
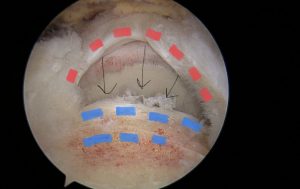
A torn rotator cuff tear at the time of surgery arthroscopically.
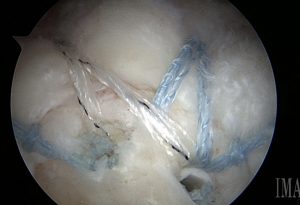
A repaired rotator cuff.
Recovery After Rotator Cuff Repair
The recovery after a rotator cuff repair is around six months. However, improvement will continue to occur up to one year after the surgery. The recovery process can be divided into three six-week phases. You will be working with a physical therapist throughout each phase. In the initial six weeks, the patient will not be able to actively raise their arm. Overtime, as you rebuild strength, you will be able to return to a wider range of motion. The last 6 week block of recovery is focused on strengthening. Of course, each person’s recovery process is different, and may vary slightly in length.
If you are seeking rotator cuff treatment and repair in the Louisville, Kentucky-area, board certified sports medicine physician Dr. Stacie Grossfeld at Orthopaedic Specialists PLLC can help. Orthopaedic Specialists PLLC is accepting new patients, and same day/telemedicine appointments are available. For additional information or to schedule an appointment, please call us at 502-212-2663.



 Meet our patient of the month Brie Postema! Brie is currently a freshman at Virginia Tech and a member of their Division 1 volleyball team!
Meet our patient of the month Brie Postema! Brie is currently a freshman at Virginia Tech and a member of their Division 1 volleyball team!
Recent Comments