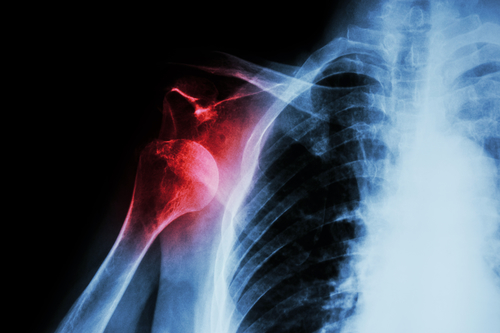
 This July, Orthopaedic Specialists is raising awareness about shoulder health through blog posts. These posts will focus on medical research regarding shoulder injuries as well as shoulder strengthening exercises and tips. If you struggle with pain and tightness in your shoulders that prevents you from living your life to the fullest, follow along for five exercises that are clinically proven to increase shoulder strength and benefit shoulder health.
This July, Orthopaedic Specialists is raising awareness about shoulder health through blog posts. These posts will focus on medical research regarding shoulder injuries as well as shoulder strengthening exercises and tips. If you struggle with pain and tightness in your shoulders that prevents you from living your life to the fullest, follow along for five exercises that are clinically proven to increase shoulder strength and benefit shoulder health.
The human shoulder consists of three bones: the clavicle (more commonly called the collarbone), the scapula (shoulder blade), and the humerus (upper arm bone), plus multiple ligaments, tendons, and muscles. These bones, tendons, ligaments, and muscles all work together as a ball and socket joint. This construction makes the shoulder one of the most mobile joints in the body. This wide range of motion makes the shoulder unstable and prone to injuries including dislocations. The proneness to injury the shoulder is subjected to means it’s pertinent to integrate shoulder strengthening exercises into your life. It isn’t necessary to have a gym membership, or even at-home gym equipment, in order to practice the following five exercises and improve your shoulder health.
5 Shoulder Strengthening Exercises that Benefit Shoulder Health
1. The Body Saw
While it sounds more like a magic trick than an exercise, the Body Saw benefits your core and scapular function. It can be performed on hardwood flooring or carpeting; however, if you do it on hard flooring than you need to wear socks and if you are working out on carpeting, you will need to place your feet on furniture moving discs. You will start out in the standard plank position and retract your shoulder blades together, so that your upper back is straightened out and not rounded. Push your body from your hands while maintaining a planking position. You will want your feet to slide about half of a foot back from the starting position. Pull your body back into the starting position and repeat for the number of reps that you choose to do.
2. “Empty the Can”
While it may sound more like a chore that you’d delegate to one of your children, this exercise is proven to work the muscles throughout your upper back and shoulders that are important in raising your arms above your head. It is recommended by Active.com to use a light weight when completing this exercise, but if you don’t have at-home weights then you can use anything from a bag of dry rice to a can of soup as a starting substitute.
To complete this exercise, you will start with your feet set apart as wide as your hips with your knees relaxed and a weight in one hand with your thumb resting against your thigh. Lift your weighted arm up until it is in a 45 degree angle from your body and rotate your thumb to point down while raising your arm. This is where the motion gets its name – your movement should mimic pouring out a can. Continue to lift your arm until it is at shoulder height, hold, then move back to the starting position.
3. The Classic: Push-Up
The push-up is a great place to start if you are looking to strengthen your shoulders, but aren’t too savvy at exercising. This simple and straightforward exercise will also help you maintain shoulder strength over time. A push-up helps to strengthen multiple areas of your body including: your triceps, shoulders and chest and strengthens them all at the same time!
Start by lying down on a mat and placing your hands where they are shoulder width apart. Get into a planking position and slowly bring your chest towards the ground using your upper body and arms. Lower your chest until it touches the ground and then push back up into the starting position. Repeat 10-20 times for 2-3 sets depending on your exercise experience.
If you are working on building shoulder strength and are not experienced in exercising – you can also do push-ups with your knees on the ground. Just make sure that your back is straight and your buttocks is low to the ground, so you do not strain your back.
4. Clasping Exercise
This is an exercise that originated from a yoga pose and is an easy shoulder strengthening exercise to complete at home, at work, or in the gym. Additionally, if you are dealing with shoulder pain, this exercise will help to alleviate that pain quickly and naturally.
To complete this exercise, start by standing up and clasping your hands behind your back. Inhale as you open up your chest and clasp your hands. Exhale as you bend forward at the waist, bringing your clasped hands up into the air. Hold this position for 4 seconds, and slightly pulse with your arms as you inhale again. Exhale and return to the standing position. Repeat for 10 reps and complete 2 or 3 sets of this exercise.
It is recommended to complete this exercise in the morning or before bed depending on when your shoulders hurt. If you suffer from tight shoulders in the morning when you wake up, try this exercise out the night before. If your shoulders start to cause you discomfort midday, the morning may be a better time to complete this exercise.
5. Shoulder Circles
Another classic exercise that will take you back to middle school gym class and is a great shoulder strengthening exercise are shoulder circles. While it may be assumed that shoulder circles do not need explanation, it is important to complete this exercise correctly and avoid injury.
Stand with your feet shoulder width apart and your knees slightly bent with your arms out and parallel to the ground. Instead of keeping your arms straight out, bend them slightly at the elbow. This helps to stave off fatigue and also concentrates the exercise on the shoulders. Once you are in this position, complete clockwise circles with your arms for 1 minute. Then reverse the direction and complete counter-clockwise circles for another minute. Repeat for 5-10 sets.
If you want to increase the difficulty of the exercise, you can alternate standing on one leg for each set. This will include your core in the workout while you try to maintain balance.
Shoulder strengthening exercises are not only important if you want to build and maintain shoulder strength. If you are recovering from a shoulder injury or shoulder surgery, shoulder strengthening exercises can benefit your recovery. As you progress in your exercise regimen, continue to encourage yourself and increase weights gradually in exercises where weights are involved. Before starting a workout regimen that involves shoulder strengthening exercises, consult your doctor. This is especially important if you are recovering from a shoulder injury or surgery.
For More Information on Shoulder Strengthening Exercises
Dr. Stacie Grossfeld is a double board-certified orthopedic surgeon in Louisville, KY with a specialty in sports medicine. She has successfully treated injured shoulders and performed shoulder surgeries for over twenty years. She commonly treats rotator cuff tears, dislocated shoulders, frozen shoulders, shoulder impingement syndrome, pitcher’s and swimmer’s shoulder injuries. Dr. Grossfeld also routinely performs rotator cuff repairs arthroscopically at both of her private practice locations. If you are suffering from shoulder pain that is not going away or you have injured your shoulder and need medical attention from an experienced orthopedic doctor, contact Dr. Grossfeld today by calling 502-212-2663.
 While eating nutritious foods and working out are great ways to improve your health, there is so much more to consider. Health and wellness requires a holistic approach that not only focuses on nutrition and fitness, but other areas as well. In order to achieve optimal health, it may be worth your while to take a look at the 15 habits of healthy people.
While eating nutritious foods and working out are great ways to improve your health, there is so much more to consider. Health and wellness requires a holistic approach that not only focuses on nutrition and fitness, but other areas as well. In order to achieve optimal health, it may be worth your while to take a look at the 15 habits of healthy people.

 Knee Osteoarthritis is a common type of arthritis that often occurs in older people, but can affect younger people, as well. Osteoarthritis of the knee is a degenerative disease that occurs when the flexible, sponge-like tissue between joints wears down. When this tissue wears down, joints no longer have padding between them and bone rubs on bone causing extreme pain. Osteoarthritis can occur in hands, the lower back area, wrists, hips, the neck, and in the knees. Quite a lot of people think that the only resolution to Knee Osteoarthritis is to take it easy on using the knees, but that is actually not true. Exercise in small, monitored doses is commonly recommended by doctors as the first approach to treating Knee Osteoarthritis.
Knee Osteoarthritis is a common type of arthritis that often occurs in older people, but can affect younger people, as well. Osteoarthritis of the knee is a degenerative disease that occurs when the flexible, sponge-like tissue between joints wears down. When this tissue wears down, joints no longer have padding between them and bone rubs on bone causing extreme pain. Osteoarthritis can occur in hands, the lower back area, wrists, hips, the neck, and in the knees. Quite a lot of people think that the only resolution to Knee Osteoarthritis is to take it easy on using the knees, but that is actually not true. Exercise in small, monitored doses is commonly recommended by doctors as the first approach to treating Knee Osteoarthritis. 
 The frequency in which concussions occur in the National Football League (NFL) is an issue of concern. In the March issue of the
The frequency in which concussions occur in the National Football League (NFL) is an issue of concern. In the March issue of the 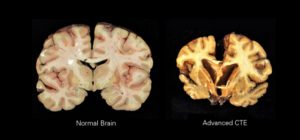 In an attempt to combat the frequency of concussions, the NFL implemented concussion management policies, and changed rules to place greater emphasis on penalizing players for aggressive behavior. However, there is still an urgent need to further strengthen policies and introduce concussion prevention and management programs.
In an attempt to combat the frequency of concussions, the NFL implemented concussion management policies, and changed rules to place greater emphasis on penalizing players for aggressive behavior. However, there is still an urgent need to further strengthen policies and introduce concussion prevention and management programs.

 ACL stands for Anterior Cruciate Ligament and this part of the human body runs between the femur and the tibia. It is one of a pair of cruciate ligaments in the human knee. The other is the Posterior Cruciate Ligament which is located deeper within the knee joint. When an ACL is injured, or torn, it is due to the ligament being overstretched. Most often,
ACL stands for Anterior Cruciate Ligament and this part of the human body runs between the femur and the tibia. It is one of a pair of cruciate ligaments in the human knee. The other is the Posterior Cruciate Ligament which is located deeper within the knee joint. When an ACL is injured, or torn, it is due to the ligament being overstretched. Most often, This July, Orthopaedic Specialists is raising awareness about shoulder health through blog posts. These posts will focus on medical research regarding shoulder injuries as well as shoulder strengthening exercises and tips. If you struggle with pain and tightness in your shoulders that prevents you from living your life to the fullest, follow along for five exercises that are clinically proven to increase shoulder strength and benefit shoulder health.
This July, Orthopaedic Specialists is raising awareness about shoulder health through blog posts. These posts will focus on medical research regarding shoulder injuries as well as shoulder strengthening exercises and tips. If you struggle with pain and tightness in your shoulders that prevents you from living your life to the fullest, follow along for five exercises that are clinically proven to increase shoulder strength and benefit shoulder health. Lyme disease is a bacterial infection that is transmitted by Ixodes ticks, more commonly known as deer ticks. These nymphal ticks are about the size of poppy seeds, yet they carry the dangerous Lyme disease in their bites. Ticks are thought of as insects, but they are actually arachnids that are related to scorpions and spiders. Deer ticks are found all over the United States and in more than 60 other countries. These ticks attach to one’s skin through questing and are able to feed for several days on one host. If left undisturbed, they are more likely to transmit Lyme disease and other pathogens into one’s bloodstream.
Lyme disease is a bacterial infection that is transmitted by Ixodes ticks, more commonly known as deer ticks. These nymphal ticks are about the size of poppy seeds, yet they carry the dangerous Lyme disease in their bites. Ticks are thought of as insects, but they are actually arachnids that are related to scorpions and spiders. Deer ticks are found all over the United States and in more than 60 other countries. These ticks attach to one’s skin through questing and are able to feed for several days on one host. If left undisturbed, they are more likely to transmit Lyme disease and other pathogens into one’s bloodstream.
Recent Comments