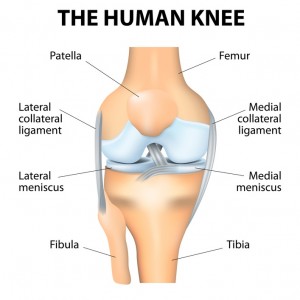
 Chronic knee pain can be debilitating and extremely frustrating, especially when it comes to physical activity. Knee pain is the result of one or many different causes. Age, injury, arthritis and excess weight can damage the cartilage inside the knee joint.
Chronic knee pain can be debilitating and extremely frustrating, especially when it comes to physical activity. Knee pain is the result of one or many different causes. Age, injury, arthritis and excess weight can damage the cartilage inside the knee joint.
Cartilage works like a cushion for your knee and over time it gets broken down. With added body weight, injuries or arthritis, your aging knee may become increasingly vulnerable to constant force.
Treating Chronic Knee Pain
Prolonged knee pain can be a long, painful injury, but there are things you can do to get some relief.
- Rest: This seems like the easiest alternative, however, staying off of your feet can be a hard task for those always on the go. By allowing your body to get some rest, your knee can take a break from constantly bearing weight. This time off allows your cartilage to strengthen and rebuild.
- Anti-Inflammatory Medication: While taking medicine for knee pain may not seem ideal, this can be an important way to help reduce inflammation and provide some pain relief. This treatment is the fairly conservative and its main goal is to help you get back on your feet.
- Ice: Icing the affected knee(s) can provide instant pain relief and also helps reduce inflammation. Icing is key for those who endure physical activity with chronic knee pain. You should apply ice to your knee at least two to three times a day for best results.
- Lose Weight: Maintaining a healthy weight can definitely help alleviate some knee pain. For those carrying extra pounds, losing weight can seem like an insurmountable challenge. Weight loss is something a lot of people struggle with and put off. In order for your knee to feel its best, a healthy weight loss program might be your best solution.
- Change Exercise: Runners and other athletes that engage in high impact sports tend to put a lot of strain and pressure on their knees. Fortunately there are several alternative exercises that will still help you maintain a high level of fitness. Try switching up your routine with non-weight bearing activities like swimming or biking.
- Physical Therapy: If your knee pain has become so severe that you need more than just rest or icing, physical therapy may be a viable option. Here, specialists can direct you with strengthening exercises and pain relieving stretches for your knee.
- Knee Surgery: This is the most serious treatment option. Any type of surgery comes with risks, so this decision should not be made lightly. After other options have been explored, surgery may be the appropriate treatment.



 to their last two – one in Vermont and the grand finale in Hawaii.
to their last two – one in Vermont and the grand finale in Hawaii.





Recent Comments