Sudden sharp pain, popping, tearing and tenderness — these are the general symptoms associated with hamstring strains. This injury can be sidelining and chronic if you do not take the appropriate precautions or steps towards rehabilitation. While most hamstring strains occur on the field or court during a soccer, football, or basketball game, they are also known to affect dancers and runners as well.
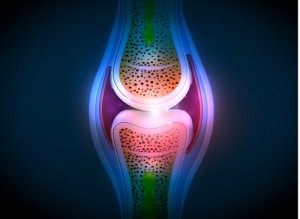
The hamstring muscles make up a group of three muscles that run up the back of your thigh to your hip bone. These strong muscles are responsible for your ability to stretch your leg directly behind your body and when bending your knee. Injury may result during physical activity if one or all of these muscles reaches its breaking point.
Treating Hamstring Strains – A Standard Approach
While most hamstring strains can be treated with home remedies by using the RICE method (Rest, Ice, Compression and Elevation), some serious injuries may require more care. If pain does not fade after following the RICE method, it might be necessary to visit a qualified physician. After a general exam and possible X-rays and MRIs, the physician will diagnose a hamstring strain. Oftentimes, the physician will suggest possible treatments including:
- Rest: Taking a break from physical or strenuous activity will give your muscles the chance they need to reduce swelling, inflammation and stress.
Support: Using crutches or a cane will help take the pressure off of the injured leg in order to advance the healing progress. - Ice: Just like the RICE method, applying ice 2-3 times a day for 10-20 minutes will help reduce the swelling in your muscles.

- Pressure: Wearing compression shorts or an ace bandage will help minimize swelling in this area.
- Elevation: Continue to rest your muscles, but do so in an elevated position. Extending your leg above your heart will give your muscles improved circulation and decreased swelling.
- Pain Medication: Taking over-the-counter pain medicine like ibuprofen or acetaminophen will help with the pain and inflammation. (more…)



 and work with the patinets together in the same room. It was so neat to be able to see all different women at different levels of medical education working together to help patients. The whole experience was incredibly empowering, and Dr. Grossfeld has truly inspired me to continue on my own path toward becoming a physician.
and work with the patinets together in the same room. It was so neat to be able to see all different women at different levels of medical education working together to help patients. The whole experience was incredibly empowering, and Dr. Grossfeld has truly inspired me to continue on my own path toward becoming a physician.  ut Bicycle Accidents – 10 Things to Know
ut Bicycle Accidents – 10 Things to Know

 cent over the last 25 years! While the number of marathon runners over age 40 has increased over the last 20-30 years, making 50 percent of all marathons older than 40-years-old.
cent over the last 25 years! While the number of marathon runners over age 40 has increased over the last 20-30 years, making 50 percent of all marathons older than 40-years-old.


Recent Comments