 If every school had an athletic trainer as dedicated, knowledgeable and passionate about their work, there’s no doubt the number of youth sports injuries would significantly drop, while the overall athletic performance would noticeably increase. But Kelly Dike is one of a kind and it’s certain that very few school athletic programs have an athletic trainer as dedicated and experienced.
If every school had an athletic trainer as dedicated, knowledgeable and passionate about their work, there’s no doubt the number of youth sports injuries would significantly drop, while the overall athletic performance would noticeably increase. But Kelly Dike is one of a kind and it’s certain that very few school athletic programs have an athletic trainer as dedicated and experienced.
Born and raised in Wisconsin, Kelly has over 12 years of experience serving the South Oldham community. She works as an employee for Baptist Sports Medicine with a full-time job at South Oldham High School.
Becoming a Certified Athletic Trainer
While many of us go through college having no idea what we really want to do for a long-term career, Kelly was fortunate. After suffering from several knee injuries in high school, she was sent to her school athletic trainer. She explains: “When I got exposed to the profession as a patient, I just realized, wow, this is really cool … this is something I’d love to do.”
 After graduating from high school, Kelly attended Winona State University in Minnesota, earning a B.S. in Exercise Science. And then she went on to Indiana State to complete her Master’s Degree. The summer before starting graduate school, Kelly landed an internship at a Lexington Sports Medicine Clinic. “I really liked Kentucky,” she explains, “and I have some extended family in Oldham County so that was definitely a location that I was interested in…” But at graduation time, there weren’t any job openings in the area, so Kelly went home to live with her parents while looking for a job. Three weeks later she was offered a position in a small school near Lansing, Michigan and off she moved.
After graduating from high school, Kelly attended Winona State University in Minnesota, earning a B.S. in Exercise Science. And then she went on to Indiana State to complete her Master’s Degree. The summer before starting graduate school, Kelly landed an internship at a Lexington Sports Medicine Clinic. “I really liked Kentucky,” she explains, “and I have some extended family in Oldham County so that was definitely a location that I was interested in…” But at graduation time, there weren’t any job openings in the area, so Kelly went home to live with her parents while looking for a job. Three weeks later she was offered a position in a small school near Lansing, Michigan and off she moved.
In the spring of 2005, Kelly saw a job opening serving South Oldham High School and she decided to apply. After a series of interviews, she was very excited to be offered the position, but would only accept under the condition that she could finish out the school year she’d already started in Michigan. She was dedicated to the athletes and the school system that she was serving and didn’t want to leave them during the middle of the school year. This is just one small example of the type of character Kelly exudes.
A Day in the Life of a Nationally Certified and State Licensed High School Athletic Trainer
Kelly’s day varies significantly depending on the time of year but one thing that remains a constant – her work is almost always busy. For example, during the summer when many educators enjoy some R&R, Kelly is immersed in preseason which kicks off July 15th. Preseason field hockey practice generally goes from 6 a.m. until 8 a.m. followed by soccer from 8 a.m. until 10 a.m. Cross country is often in the morning too, and then around 2 p.m. in the afternoon football starts. (more…)

 Dr. Stacie Grossfeld is a double board-certified surgeon in the fields of orthopedic surgery and also sports medicine. Her combination of specialties means that she spends a lot of time working with injured athletes around Louisville, KY. One of the most common injuries among high school and college athletes are torn Anterior Cruciate Ligaments (ACLs). In order to offer the best medical care that she can, Dr. Grossfeld stays up-to-date on scientific findings surrounding
Dr. Stacie Grossfeld is a double board-certified surgeon in the fields of orthopedic surgery and also sports medicine. Her combination of specialties means that she spends a lot of time working with injured athletes around Louisville, KY. One of the most common injuries among high school and college athletes are torn Anterior Cruciate Ligaments (ACLs). In order to offer the best medical care that she can, Dr. Grossfeld stays up-to-date on scientific findings surrounding  Ironman Louisville takes place this weekend and competitors from all over the world will be present to participate. The Ironman Louisville is a qualifier for the Kona Ironman World Championship held on the Big Island of Hawaii every year.
Ironman Louisville takes place this weekend and competitors from all over the world will be present to participate. The Ironman Louisville is a qualifier for the Kona Ironman World Championship held on the Big Island of Hawaii every year. The finalists for Louisville Business First’s 2017 Business of the Year Awards have been released.
The finalists for Louisville Business First’s 2017 Business of the Year Awards have been released. It is a common misconception that sodium is bad for you. While excessive sodium levels can be dangerous and put you at a risk for certain health issues, your body needs sodium. Sodium is on the periodic table of elements and is an electrolyte. When the right amount of sodium is in the body, it helps to regulate water levels in your cells. However, when too much sodium or not enough is in the body, complications can arise. When the sodium levels in the body are too low, cells start to swell. Swelling cells can cause a wide range of health problems that range from mild to life-threatening. Hyponatremia is a result of not having enough sodium in the body. Whether the cause of lowered sodium levels is a medical condition or from consuming too much water, hyponatremia can occur.
It is a common misconception that sodium is bad for you. While excessive sodium levels can be dangerous and put you at a risk for certain health issues, your body needs sodium. Sodium is on the periodic table of elements and is an electrolyte. When the right amount of sodium is in the body, it helps to regulate water levels in your cells. However, when too much sodium or not enough is in the body, complications can arise. When the sodium levels in the body are too low, cells start to swell. Swelling cells can cause a wide range of health problems that range from mild to life-threatening. Hyponatremia is a result of not having enough sodium in the body. Whether the cause of lowered sodium levels is a medical condition or from consuming too much water, hyponatremia can occur.  Pregnancy is a miracle in and of itself; however, that doesn’t mean that the entire process is painless. For most women, the excitement of bringing a child into the world overpowers any discomfort. That is not the case for everyone though. Some women find themselves in quite a bit of pain while pregnant. One of the most common causes of pain in women who are pregnant is backache. Other causes of pain and discomfort include:
Pregnancy is a miracle in and of itself; however, that doesn’t mean that the entire process is painless. For most women, the excitement of bringing a child into the world overpowers any discomfort. That is not the case for everyone though. Some women find themselves in quite a bit of pain while pregnant. One of the most common causes of pain in women who are pregnant is backache. Other causes of pain and discomfort include: Imagine a young athlete at the top of his game– perhaps a cyclist. He works out daily, eats right, and gets plenty of rest. He is visibly healthy in every way with no familial history of cardiovascular disease. Yet this young man could be at risk for arterial disease… but why?
Imagine a young athlete at the top of his game– perhaps a cyclist. He works out daily, eats right, and gets plenty of rest. He is visibly healthy in every way with no familial history of cardiovascular disease. Yet this young man could be at risk for arterial disease… but why? 

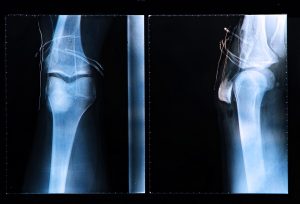 A torn Anterior Cruciate Ligament, more commonly known as an ACL, can be a difficult injury for a high school or college athlete to sustain. Unfortunately, they are also the most common injuries sustained by athletes. Football, soccer, hockey, and basketball players are highly likely to sustain an ACL injury over their athletic career and ACL injuries are becoming more common thanks to a variety of factors including:
A torn Anterior Cruciate Ligament, more commonly known as an ACL, can be a difficult injury for a high school or college athlete to sustain. Unfortunately, they are also the most common injuries sustained by athletes. Football, soccer, hockey, and basketball players are highly likely to sustain an ACL injury over their athletic career and ACL injuries are becoming more common thanks to a variety of factors including:
Recent Comments